Therapists’ Lived Experience of Empathic Fatigue and Professional Identity
Keywords:
Empathic fatigue, professional identity, mental health therapists, Kenya, emotional exhaustion, coping strategiesAbstract
Objective: The objective of this study was to explore the lived experiences of empathic fatigue and its impact on professional identity among therapists in Kenya.
Methods and Materials: This qualitative research employed a phenomenological approach to understand the emotional and professional implications of empathic fatigue. Semi-structured interviews were conducted with 25 therapists from Kenya who had varying levels of experience in mental health practice. Data were analyzed using thematic analysis with NVivo software to identify emerging themes and subthemes, with theoretical saturation guiding the conclusion of data collection.
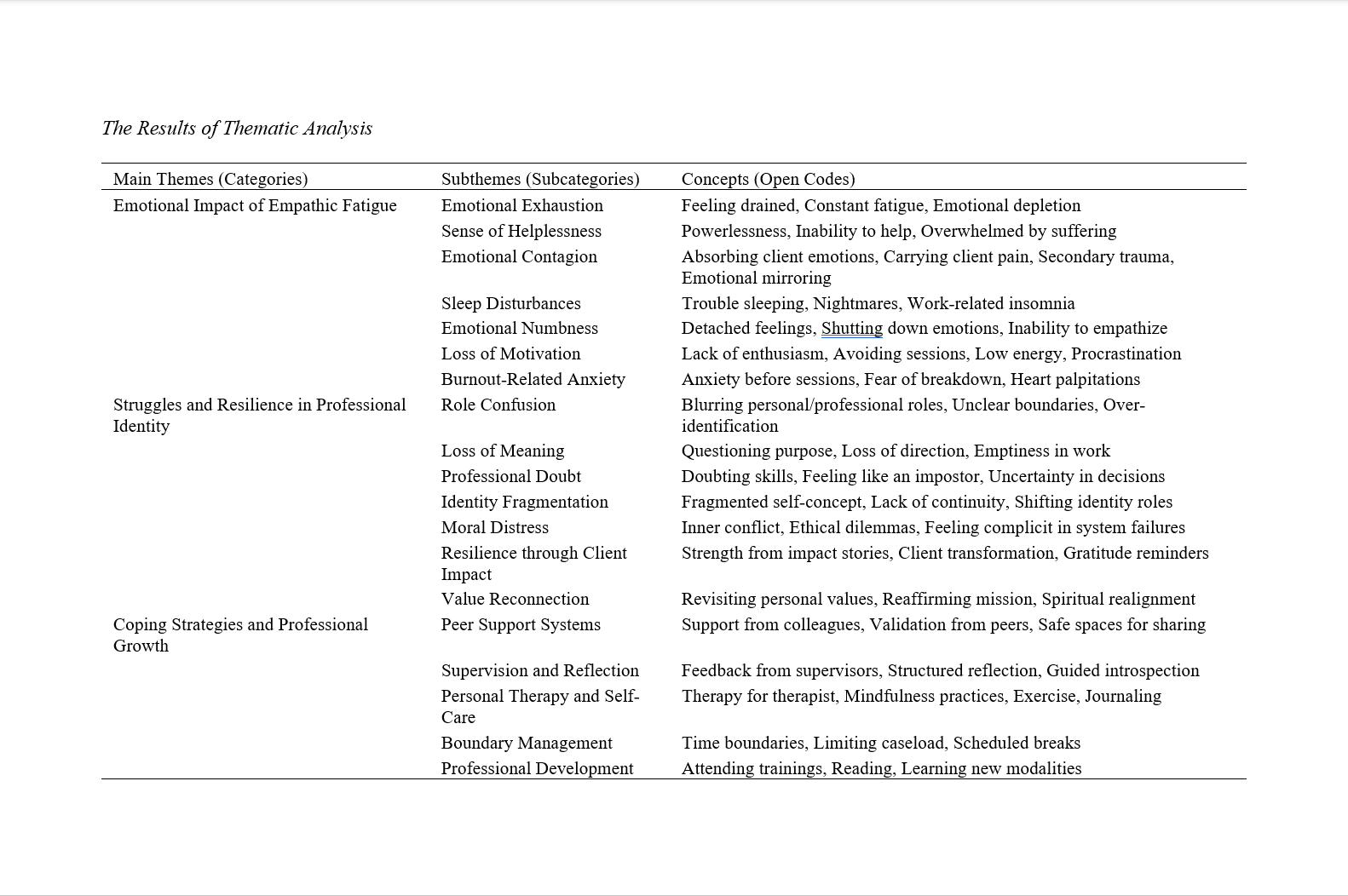
Findings: The findings revealed three main themes: emotional impact of empathic fatigue, struggles and resilience in professional identity, and coping strategies and professional growth. Participants reported experiencing emotional exhaustion, emotional contagion, and sleep disturbances. These were accompanied by identity-related challenges, including role confusion, identity fragmentation, and loss of professional meaning. Despite these challenges, therapists demonstrated resilience through client impact and professional growth. Key coping strategies included peer support, supervision, personal therapy, and self-care practices.
Conclusion: This study highlights the complex interplay between empathic fatigue and professional identity among therapists in Kenya. While empathic fatigue poses significant emotional and professional challenges, therapists also exhibit adaptive responses that foster resilience and renewal. The findings suggest the need for institutional support systems and self-care practices to mitigate the impact of empathic fatigue.
Downloads
References
Anandan, R., Cross, W., & Olasoji, M. (2024). Mental Health Nurses' Empathy Experiences Towards Consumers With Dual Diagnosis: A Thematic Analysis. Journal of Psychiatric and Mental Health Nursing, 31(5), 904-915. https://doi.org/10.1111/jpm.13039
Bartels‐Velthuis, A. A., Brink, E. v. d., Koster, F., & Hoenders, R. (2020). The Interpersonal Mindfulness Program for Health Care Professionals: A Feasibility Study. Mindfulness, 11(11), 2629-2638. https://doi.org/10.1007/s12671-020-01477-5
Bell, S. A., Hopkin, G., & Forrester, A. (2019). Exposure to Traumatic Events and the Experience of Burnout, Compassion Fatigue and Compassion Satisfaction Among Prison Mental Health Staff: An Exploratory Survey. Issues in Mental Health Nursing, 40(4), 304-309. https://doi.org/10.1080/01612840.2018.1534911
Cardoso, A. A., Tomotani, D. Y. V., & Mucci, S. (2023). Compassion Fatigue and Coping Strategies Before Death. Revista Bioética, 31. https://doi.org/10.1590/1983-803420233271en
Chang, J.-J., & Shin, S. H. (2021). A Path Model for Burnout in Community Mental Health Professionals. International journal of environmental research and public health, 18(18), 9763. https://doi.org/10.3390/ijerph18189763
DeDiego, A. C., Farrell, I. C., Basma, D., & Maurya, R. K. (2024). Impact of Immigration and Discrimination on Vocational Wellness for Immigrant Mental Health Professionals. Journal of employment counseling, 61(2), 118-135. https://doi.org/10.1002/joec.12222
Erbe, A. M. (2022). Compassion Fatigue and Mental Health in Health Care Professionals. Workplace Health & Safety, 70(6), 303-303. https://doi.org/10.1177/21650799221081237
Fernández, M. D. R., Ramos‐Pichardo, J. D., Ibáñez‐Masero, O., Carmona‐Rega, M. I., Sánchez-Ruiz, M. J., & Ortega‐Galán, Á. M. (2021). Professional Quality of Life, Self‐compassion, Resilience, and Empathy in Healthcare Professionals During COVID‐19 Crisis in Spain. Research in Nursing & Health, 44(4), 620-632. https://doi.org/10.1002/nur.22158
Free, G., Swildens, W., Knapen, S., Beekman, A. T., & Meijel, B. v. (2023). Mentalizing Capacities of Mental Health Nurses: A Systematic PRISMA Review. Journal of Psychiatric and Mental Health Nursing, 31(1), 87-110. https://doi.org/10.1111/jpm.12963
Hobeika, E., Hallit, S., Sacre, H., Obeïd, S., Hajj, A., & Salameh, P. (2020). Factors Associated With Empathy Among Community Pharmacists in Lebanon. Journal of Pharmaceutical Policy and Practice, 13(1). https://doi.org/10.1186/s40545-020-00237-z
Kabunga, A., Apio, B., & Anyolitho, M. K. (2019). Emotional Intelligence as Predictor of Compassion Fatigue Among Mental Health Practitioners. Oalib, 06(05), 1-10. https://doi.org/10.4236/oalib.1105410
Kinman, G., & Grant, L. (2020). Emotional Demands, Compassion and Mental Health in Social Workers. Occupational Medicine, 70(2), 89-94. https://doi.org/10.1093/occmed/kqz144
Kinman, G., Grant, L., & Kelly, S. (2019). ‘It’s My Secret Space’: The Benefits of Mindfulness for Social Workers. The British Journal of Social Work, 50(3), 758-777. https://doi.org/10.1093/bjsw/bcz073
Kounenou, K., Kalamatianos, A., Nikoltsiou, P., & Kourmousi, N. (2023). The Interplay Among Empathy, Vicarious Trauma, and Burnout in Greek Mental Health Practitioners. International journal of environmental research and public health, 20(4), 3503. https://doi.org/10.3390/ijerph20043503
López‐López, I. M., Gómez-Urquiza, J. L., Cañadas, G. R., Fuente, E. I. D. L., Albendín‐Garcia, L., & Guillermo, A. C. D. l. F. (2019). Prevalence of Burnout in Mental Health Nurses and Related Factors: A Systematic Review and Meta‐analysis. International journal of mental health nursing, 28(5), 1035-1044. https://doi.org/10.1111/inm.12606
Mantelou, A., & Karakasidou, E. (2019). The Role of Compassion for Self and Others, Compassion Fatigue and Subjective Happiness on Levels of Well-Being of Mental Health Professionals. Psychology, 10(03), 285-304. https://doi.org/10.4236/psych.2019.103021
Pérez-Chacón, M., Chacón, A., María de las Mercedes Borda, M., & Navarro, M. L. A. (2021). Sensory Processing Sensitivity and Compassion Satisfaction as Risk/Protective Factors From Burnout and Compassion Fatigue in Healthcare and Education Professionals. International journal of environmental research and public health, 18(2), 611. https://doi.org/10.3390/ijerph18020611
Rashid, Z., Sharif, I., Khushk, I. A., & Raja, A. A. (2021). Evaluation of Empathy and Fatigue Among Physicians and Surgeons in Tertiary Care Hospitals of Rawalpindi. Pakistan Journal of Medical Sciences, 37(3). https://doi.org/10.12669/pjms.37.3.1973
Raynor, D., & Hicks, R. E. (2018). Empathy and Coping as Predictors of Professional Quality of Life in Australian Registered Migration Agents (RMAs). Psychiatry Psychology and Law, 26(4), 530-540. https://doi.org/10.1080/13218719.2018.1507846
Sattar, K., Yusoff, M. S. B., Arifin, W. N., Yasin, M. A. M., & Nor, M. Z. M. (2023). A Scoping Review on the Relationship Between Mental Wellbeing and Medical Professionalism. Medical Education Online, 28(1). https://doi.org/10.1080/10872981.2023.2165892
Shoji, K., Noguchi, N., Waki, F., Saito, T., Kitano, M., Edo, N., Koga, M., Toda, H., Kobayashi, N., Sawamura, T., & Nagamine, M. (2024). Empathy and Coping Strategies Predict Quality of Life in Japanese Healthcare Professionals. Behavioral Sciences, 14(5), 400. https://doi.org/10.3390/bs14050400
Singh, J., Karanika‐Murray, M., Baguley, T., & Hudson, J. (2020). A Systematic Review of Job Demands and Resources Associated With Compassion Fatigue in Mental Health Professionals. International journal of environmental research and public health, 17(19), 6987. https://doi.org/10.3390/ijerph17196987
Thaís Andréa de Oliveira, M., Liniker, S., Gonçalves, R., Santana, T. P. D., Rubiane Gouveia de Souza e, S., Talita, C., Canhoto, S., Andreto, L. M., Beatriz, M., Pinto, F., Sousa, C., Silva, J. D., Claudino, D., Mariane, J., Cavalcante, S., Wanessa, M., Arlen, D., Marcos César de Oliveira, S., Scolfild, L., & Silva, R. d. (2022). Engagement and Empathy of Health Professionals Working to Combat Covid-19 in Pernambuco. International Journal of Development Research, 59155-59159. https://doi.org/10.37118/ijdr.25420.09.2022
Venner, M. (2024). An Exploration of Empathy Fatigue in Counsellors and Their Use of Self-Care Strategies. https://doi.org/10.21203/rs.3.rs-4258196/v1
Yu, C. C., Tan, L., Le, M. K., Tang, B., Liaw, S. Y., Tierney, T., Ho, Y. Y., Lim, B. E. E., Daphne, A. F. N. L., Ng, R., Chia, S. C., & Low, J. A. (2022). The Development of Empathy in the Healthcare Setting: A Qualitative Approach. BMC Medical Education, 22(1). https://doi.org/10.1186/s12909-022-03312-y
Zhang, L., Ren, Z., Guangrong, J., Hazer-Rau, D., Zhao, C., Shi, C., Lai, L., & Yan, Y. (2021). Self-Oriented Empathy and Compassion Fatigue: The Serial Mediation of Dispositional Mindfulness and Counselor’s Self-Efficacy. Frontiers in psychology, 11. https://doi.org/10.3389/fpsyg.2020.613908
Zhao, Y., Wang, X., & Liu, T. (2024). Correlations Between Empathy Fatigue, Occupational Identity, and Sleep Quality in Nursing Staff: A Cross-Sectional Study. Frontiers in Public Health, 12. https://doi.org/10.3389/fpubh.2024.1401044
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.