The Impact of Cognitive-Behavioral Therapy on Enhancing Self-Control and Reducing Anger among Individuals Recovered from COVID-19
Keywords:
cognitive-behavioral therapy, self-control, anger, COVID-19Abstract
Abstract
Objective: The COVID-19 pandemic not only poses physical health challenges but also has significant psychological implications. This study aimed to examine the effectiveness of cognitive-behavioral therapy (CBT) in enhancing self-control and reducing anger among individuals recovered from COVID-19.
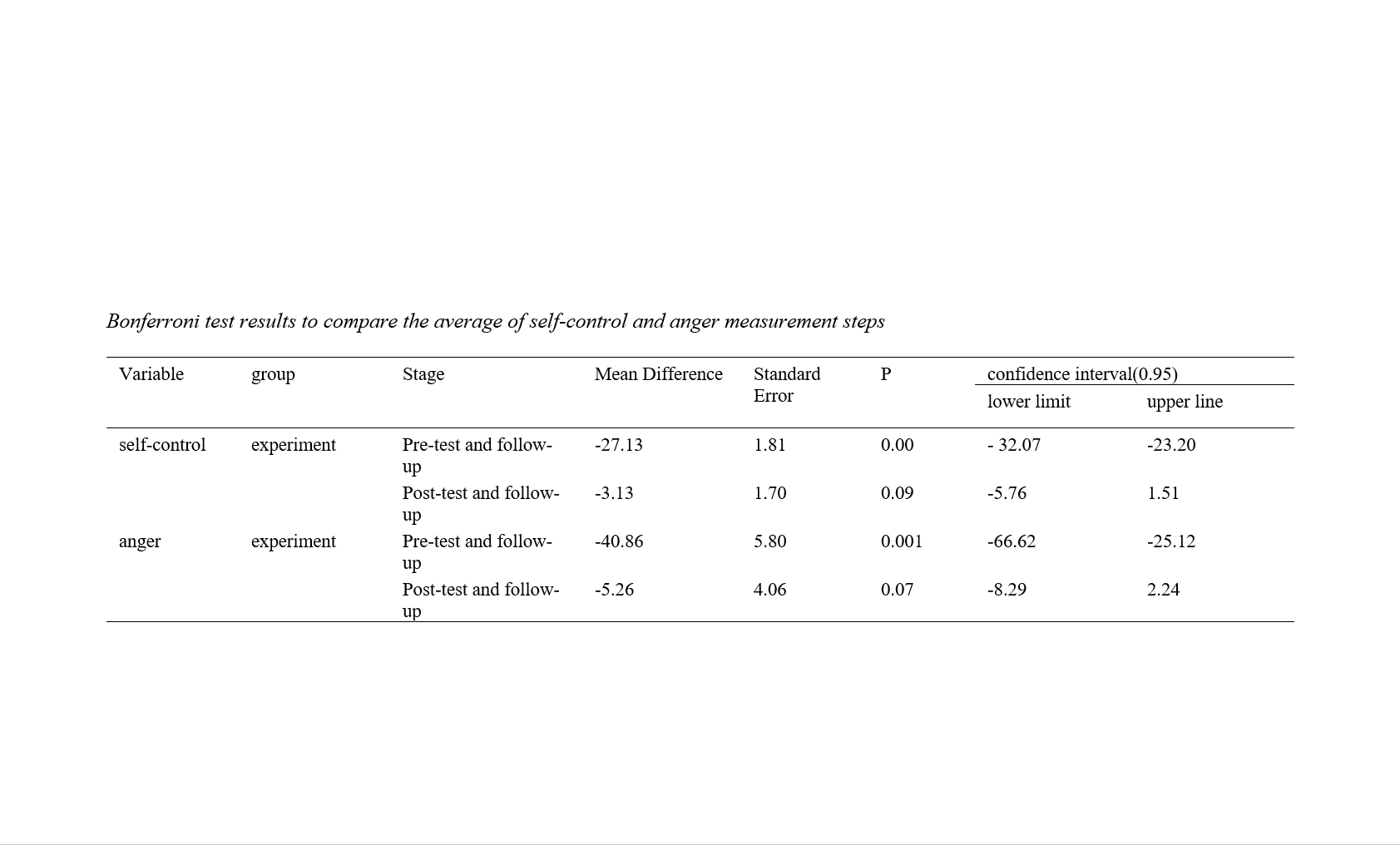
Method: A quasi-experimental design with pre-test, post-test, and follow-up assessments and a control group was used. The study population included individuals diagnosed with COVID-19 who sought treatment at [MASKED FOR REVIEW], Iran. A total of 30 participants were selected through convenient sampling and randomly assigned to either an experimental group (n = 15) or a control group (n = 15). The experimental group received nine sessions of CBT, while the control group received no intervention. Data were collected using Tanji's (1999) Self-Control Questionnaire and Buss and Perry's (1992) Aggression Questionnaire. Data analysis was conducted using analysis of covariance (ANCOVA) and repeated measures ANOVA to evaluate treatment sustainability.
Findings: The results indicated that CBT significantly improved self-control and reduced anger among individuals recovered from COVID-19.
Conclusion: CBT appears to be an effective intervention for enhancing self-control and reducing anger in individuals who have recovered from COVID-19.
Downloads
References
Alavi, S. S., Ghanizadeh, M., Mohammadi, M. R., Jannatifard, F., Esmaili Alamuti, S., & Farahani, M. (2021). The effects of cognitive-behavioral group therapy for reducing symptoms of internet addiction disorder and promoting quality of life and mental health. Trends in psychiatry and psychotherapy, 43, 47-56.
Asanjarani, F., Kumar, A., & Kalani, S. (2023). Student subjective wellbeing amidst the covid-19 pandemic in Iran: Role of loneliness, resilience and parental involvement. Child Indicators Research, 16(1), 53-67.
Asanjarani, F., Szczygieł, M., & Arif, A. (2021). The Persian language version of the obsession with the COVID-19 scale for adolescents. Frontiers in psychiatry, 12, 800982.
Asanjarani, F., & Zarebahramabadi, M. (2021). Evaluating the effectiveness of cognitive-behavioral therapy on math self-concept and math anxiety of elementary school students. Preventing School Failure: Alternative Education for Children and Youth, 65(3), 223-229.
Bonazza, F., Luridiana Battistini, C., Fior, G., Bergamelli, E., Wiedenmann, F., D’Agostino, A., Sferrazza Papa, G. F., Borghi, L., Piscopo, K., & Vegni, E. (2022). Recovering from COVID-19: psychological sequelae and post-traumatic growth six months after discharge. European journal of psychotraumatology, 13(1), 2095133.
Clemente-Suárez, V. J., Dalamitros, A. A., Beltran-Velasco, A. I., Mielgo-Ayuso, J., & Tornero-Aguilera, J. F. (2020). Social and psychophysiological consequences of the COVID-19 pandemic: An extensive literature review. Frontiers in psychology, 11, 3077.
Driessen, E., & Hollon, S. D. (2010). Cognitive behavioral therapy for mood disorders: efficacy, moderators and mediators. Psychiatric Clinics, 33(3), 537-555.
Duckworth, A. L., Milkman, K. L., & Laibson, D. (2018). Beyond willpower: Strategies for reducing failures of self-control. Psychological Science in the Public Interest, 19(3), 102-129.
Fathi Ashtiani, A., Rahnejat, A. M., Ahmadi Tahour Soltani, M., Taghva, A., Ebrahimi, M. R., Donyavi, V., & Jahandari, P. (2020). Psychological consequences and interventions during the COVID-19 pandemic: narrative review. Journal of Marine Medicine, 2(1), 1-11.
Fiorillo, A., & Gorwood, P. (2020). The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. European Psychiatry, 63(1), e32, Article e32. https://doi.org/10.1192/j.eurpsy.2020.35
Hofmann, W., Luhmann, M., Fisher, R. R., Vohs, K. D., & Baumeister, R. F. (2014). Yes, but are they happy? Effects of trait self‐control on affective well‐being and life satisfaction. Journal of personality, 82(4), 265-277.
Kunzler, L. S., Naves, L. A., & Casulari, L. A. (2018). Cognitive-behavioral therapy improves the quality of life of patients with acromegaly. Pituitary, 21, 323-333.
Lange, K. W. (2021). Coronavirus disease 2019 (COVID-19) and global mental health. Global health journal, 5(1), 31-36. https://doi.org/10.1016/j.glohj.2021.02.004
Liyanage-Don, N. A., Cornelius, T., Sanchez, J. E., Trainor, A., Moise, N., Wainberg, M., & Kronish, I. M. (2021). Psychological distress, persistent physical symptoms, and perceived recovery after COVID-19 illness. Journal of General Internal Medicine, 36(8), 2525-2527.
Macmillan, R. (2001). Violence and the life course: The consequences of victimization for personal and social development. Annual review of sociology, 27(1), 1-22.
Moeller, T. G. (2001). Youth aggression and violence: A psychological approach. Routledge.
Peterman, A., Potts, A., O'Donnell, M., Thompson, K., Shah, N., Oertelt-Prigione, S., & Van Gelder, N. (2020). Pandemics and violence against women and children (Vol. 528). Center for Global Development Washington, DC. https://cgdev.org/sites/default/files/pandemics-and-vawg-april2.pdf
Sadri Damirchi, E., & Aghazadehasl, M. (2018). The effectiveness of cognitive-behavioral group therapy on coping and self-control styles in multiple sclerosis patients. Armaghane Danesh, 22(6), 792-803.
Smith, L. E., Duffy, B., Moxham-Hall, V., Strang, L., Wessely, S., & Rubin, G. J. (2021). Anger and confrontation during the COVID-19 pandemic: a national cross-sectional survey in the UK. Journal of the Royal Society of Medicine, 114(2), 77-90.
Sood, S. (2020). Psychological effects of the Coronavirus disease-2019 pandemic. Research & Humanities in Medical Education, 7(11), 23-26.
Sun, N., Wei, L., Wang, H., Wang, X., Gao, M., Hu, X., & Shi, S. (2021). Qualitative study of the psychological experience of COVID-19 patients during hospitalization. Journal of affective disorders, 278, 15-22.
Tangney, J. P., Boone, A. L., & Baumeister, R. F. (2018). High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. In Self-regulation and self-control (pp. 173-212). Routledge.
Wood, L., Baumler, E., Schrag, R. V., Guillot-Wright, S., Hairston, D., Temple, J., & Torres, E. (2021). “Don’t know where to go for help”: Safety and economic needs among violence survivors during the COVID-19 pandemic. Journal of family violence, 1-9.
Zhao, J., Meng, G., Sun, Y., Xu, Y., Geng, J., & Han, L. (2021). The relationship between self-control and procrastination based on the self-regulation theory perspective: The moderated mediation model. Current Psychology, 40, 5076-5086.
Zsido, A. N., Arato, N., Inhof, O., Matuz-Budai, T., Stecina, D. T., & Labadi, B. (2022). Psychological well-being, risk factors, and coping strategies with social isolation and new challenges in times of adversity caused by the COVID-19 pandemic. Acta Psychologica, 225, 103538.
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2026 Sahar Khanjani Veshki (Corresponding Author); Mehdi molaei yasavoli, Parisa Saghebi (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.