Psychological Interventions and Grief-Related Protocols for Infertile Couples with a History of Spontaneous and Recurrent Miscarriage: A Systematic Review
Keywords:
Abortion, Habitual, Infertility, Psychological Intervention, Grief, Quality of Life Recurrent miscarriage, Psychological interventions, Quality of lifeAbstract
Objective: The primary aim was to synthesize evidence on the effectiveness of psychological interventions and grief protocols for infertile couples or women with spontaneous and recurrent miscarriage. Secondary aims included identifying intervention types, evaluating reported outcomes, and exploring factors affecting effectiveness.
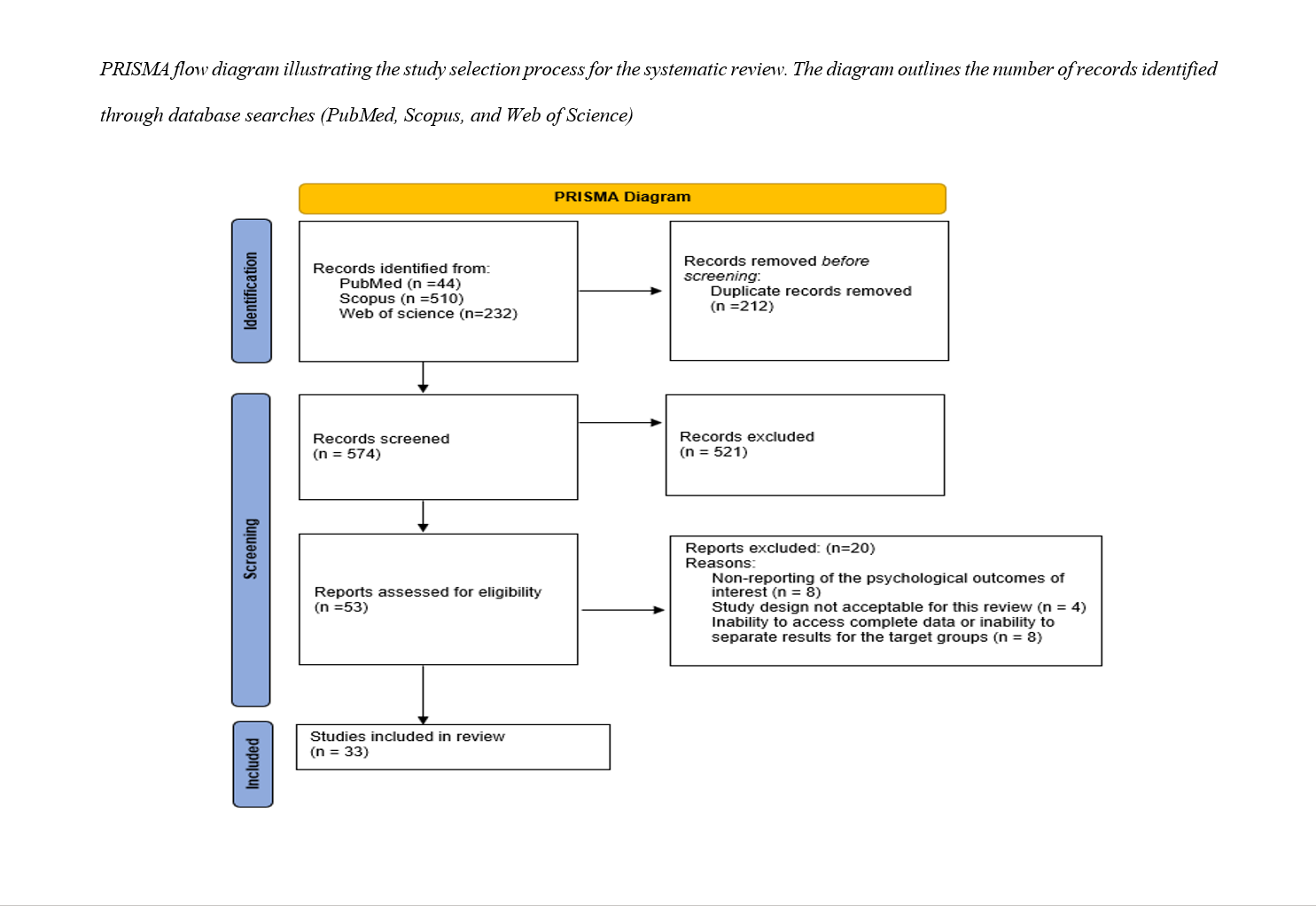
Materials and Methods: PubMed, Scopus, and Web of Science (Core Collection) were searched from inception to June 1, 2025. Eligible studies included randomized controlled trials, cohort, cross-sectional studies, and service evaluations on psychological interventions or grief protocols. Study quality was assessed using RoB 2 for RCTs and CASP for qualitative studies. Due to heterogeneity, findings were narratively synthesized.
Findings: Thirty-three studies were analyzed, evaluating approaches such as Interpersonal Psychotherapy (IPT), Cognitive Behavioral Therapy (CBT), brief supportive psychotherapy, Swanson’s Caring Theory-based counseling, art therapy, positive self-talk, and peer support. Sample sizes ranged from 14 to 932 participants, with follow-ups from immediate post-intervention to 14 months. Overall, interventions reduced anxiety, depression, and grief, and improved quality of life. Effectiveness varied by intervention timing and participant characteristics, including baseline distress and provision of medical information.
Conclusion: Psychological interventions can significantly alleviate the mental health burden following EPL. Early screening and integrated medical-psychological care are recommended. Further robust research is needed to define optimal strategies.
Downloads
References
Adolfsson, A., Berterö, C., & Larsson, P. G. (2006). Effect of a structured follow-up visit to a midwife on women with early miscarriage: a randomized study. Acta Obstetricia et Gynecologica Scandinavica, 85(3), 330-335. https://doi.org/10.1080/00016340500539376
Adolfsson, A., & Larsson, P. (2010). Applicability of general grief theory to Swedish women's experience after early miscarriage, with factor analysis of Bonanno's taxonomy, using the Perinatal Grief Scale. Upsala Journal of Medical Sciences, 115(3), 201-209. https://doi.org/10.3109/03009731003739851
Altaf Dar, M., Maqbool, M., Ara, I., & Zehravi, M. (2023). The intersection of technology and mental health: enhancing access and care. International Journal of Adolescent Medicine and Health, 35(5), 423-428. https://doi.org/10.1515/ijamh-2023-0113
Anderson, M., Gluckman, G., Ajith, T., Kirk, E., & Memtsa, M. (2024). Service evaluation of an early pregnancy loss support clinic in an inner London early pregnancy unit. BMC Health Services Research, 24(1), 123. https://doi.org/10.1186/s12913-024-11750-1
Areas, B. C. (2024). Treatment, intervention, prevention. In EPPP Step One Exam Review: Comprehensive Review, plus 450 Questions Based on the Latest Exam Blueprint.
Bagheri, L., Chaman, R., Ghiasi, A., & Motaghi, Z. (2023). Cognitive behavioral counselling in post abortion grief: A randomized controlled trial. Journal of education and health promotion, 12, 104. https://doi.org/10.4103/jehp.jehp_474_22
Bailey, S., Bailey, C., Boivin, J., Cheong, Y., Reading, I., & Macklon, N. (2015). A feasibility study for a randomised controlled trial of the Positive Reappraisal Coping Intervention, a novel supportive technique for recurrent miscarriage. BMJ open, 5(11), e009346. https://doi.org/10.1136/bmjopen-2014-007322
Barat, S., Yazdani, S., Faramarzi, M., Khafri, S., Darvish, M., Rad, M. N., & Asnafi, N. (2020). The Effect of Brief Supportive Psychotherapy on Prevention of Psychiatric Morbidity in Women with Miscarriage: A Randomized Controlled Trial about the First 24-hours of Hospitalization. Oman Medical Journal, 35(6), e197. https://doi.org/10.5001/omj.2020.48
Barbe, C., Boiteux-Chabrier, M., Charillon, E., Bouazzi, L., Maheas, C., Merabet, F., Graesslin, O., Auer, J., Hammami, S., Rolland, A. C., & Hurtaud, A. (2023). Utility of early, short psychological care for women who experience early miscarriage: protocol for the randomized, controlled MisTher trial. BMC psychology, 11(1), 198. https://doi.org/10.1186/s40359-023-01421-x
Bramble, E. A. (2024). Integrating clinical psychologists into obstetrics and gynecology settings to treat perinatal grief following miscarriage: a comprehensive literature review The Chicago School of Professional Psychology]. Chicago (IL). https://www.proquest.com/openview/a9f32e1c8d2099d85904b6f2e3cf33c9/1?pq-origsite=gscholar&cbl=18750&diss=y
Chang, S. C., Kuo, P. L., & Chen, C. H. (2021). Effectiveness of empathic caring on stress and depression for women with recurrent miscarriage: A randomized controlled trial. Complementary Therapies in Clinical Practice, 44, 101404. https://doi.org/10.1016/j.ctcp.2021.101367
Diamond, R. M., & Roose, R. E. (2016). Development and Evaluation of a Peer Support Program for Parents Facing Perinatal Loss. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 45(6), 905-914. https://pubmed.ncbi.nlm.nih.gov/27067931/
Fernlund, A., Jokubkiene, L., Sladkevicius, P., Valentin, L., & Sjöström, K. (2021). Psychological impact of early miscarriage and client satisfaction with treatment: comparison between expectant management and misoprostol treatment in a randomized controlled trial. Ultrasound in Obstetrics & Gynecology, 58(3), 420-428. https://doi.org/10.1002/uog.23641
Funston, G., O'Flynn, H., Ryan, N. A., Hamilton, W., & Crosbie, E. J. (2018). Recognizing gynecological cancer in primary care: risk factors, red flags, and referrals. Advances in Therapy, 35(4), 577-589. https://doi.org/10.1007/s12325-018-0683-3
Golmakani, N., Ahmadi, M., Asghari, P., & Esmaili, H. (2017). The effect of supportive care program on bereavement in women with early miscarriage. Iranian Journal of Obstetrics, Gynecology and Infertility, 20(5), 9-17. https://ijogi.mums.ac.ir/article_9588.html
Hori, S., Nakano, Y., Yamada, A., Azuma, H., Noda, Y., Sugiura, M., Aoki, K., Kitamura, T., & Furukawa, T. A. (2002). Personality, social support, coping and emotional distress after repeated spontaneous abortions. Journal of Psychosomatic Obstetrics & Gynecology, 23(3), 157-164. https://doi.org/10.3109/01674820209042795
Johnson, J. E., Price, A. B., Kao, J. C., Fernandes, K., Stout, R., Gobin, R., & Zlotnick, C. (2016). Interpersonal Psychotherapy (IPT) for Major Depression Following Perinatal Loss: A pilot randomized controlled trial. Archives of Women's Mental Health, 19(5), 867-872. https://doi.org/10.1007/s00737-016-0625-5
Johnson, J. E., Price, A. B., Sikorskii, A., Key, K. D., Taylor, B., Lamphere, S., Huff, C., Cinader, M., & Zlotnick, C. (2022). Protocol for the Healing After Loss (HeAL) Study: a randomised controlled trial of interpersonal psychotherapy (IPT) for major depression following perinatal loss. BMJ open, 12(9), e063025. https://doi.org/10.1136/bmjopen-2021-057747
Johnson, O. P., & Langford, R. W. (2010). Proof of Life: A Protocol for Pregnant Women Who Experience Pre-20-Week Perinatal Loss. Critical Care Nursing Quarterly, 33(3), 221-226. https://doi.org/10.1097/CNQ.0b013e3181e65f3b
Kersting, A., Dölemeyer, R., Steinig, J., Walter, F., Kroker, K., Baust, K., & Wagner, B. (2013). Brief Internet-Based Intervention Reduces Posttraumatic Stress and Prolonged Grief in Parents after the Loss of a Child during Pregnancy: A Randomized Controlled Trial. Psychotherapy and psychosomatics, 82(6), 372-381. https://doi.org/10.1159/000348713
Kersting, A., Dölemeyer, R., Wagner, B., & Linde, K. (2017). Abschied am Beginn des Lebens Behandlung spezifischer Trauersymptome nach dem Verlust eines Kindes. Psychotherapeut, 62(3), 199-206. https://doi.org/10.1007/s00278-017-0221-9
Kersting, A., Kroker, K., Schlicht, S., Baust, K., & Wagner, B. (2011). Efficacy of cognitive behavioral internet-based therapy in parents after the loss of a child during pregnancy: pilot data from a randomized controlled trial. Archives of Women's Mental Health, 14(6), 465-474. https://doi.org/10.1007/s00737-011-0240-4
Kheirkhah, M., Kiani, Z., Kianimoghadam, A. S., Amanollahi, Z., Farshad, F., & Maadi Esfahan, M. (2024). Effect of Supportive Counseling Based on Swanson's Caring Theory on the Quality of Life of Pregnant Women With A History of Abortion: A Randomized Controlled Trial Study. Iranian Journal of Psychiatry and Clinical Psychology, 30(2), 164-175. https://doi.org/10.32598/ijpcp.29.4.4131.2
Kong, G. W. S., Chung, T. K. H., & Lok, I. H. (2014). The impact of supportive counselling on women's psychological wellbeing after miscarriage-a randomised controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology, 121(3), 362-370. https://doi.org/10.1111/1471-0528.12908
Kuse-Isingschulte, M. W., Beutel, M., Hahlweg, B. C., Stauber, M., & Schneider, K. (1996). Die psychische Verarbeitung einer Totgeburt Verlauf der Trauerreaktion, Einflußfaktoren, Behandlungszufriedenheit, Betreuungswünsche. Geburtshilfe und Frauenheilkunde, 56(6), 347-352. https://doi.org/10.1055/s-2007-1023271
Li, G., Jiang, Z., Han, X., Shang, X., Tian, W., Kang, X., & Fang, M. (2020). A moderated mediation model of perceived stress, negative emotions and mindfulness on fertility quality of life in women with recurrent pregnancy loss. Quality of Life Research, 29(3), 697-708. https://doi.org/10.1007/s11136-020-02460-2
Maagh, L. C. S., Quinlan, E., Vicary, S., Schilder, S., & Carey, C. (2023). Self-compassion and Mental Health in Australian Women Who Have Experienced Pregnancy Loss. Illness, Crisis & Loss, 31(4), 991-1005. https://doi.org/10.1177/10541373221150326
Markin, R. D. (2024). Psychotherapy for pregnancy loss: applying relationship science to clinical practice. Oxford University Press. https://doi.org/10.1093/oso/9780197693353.001.0001
Murphy, F. A., Lipp, A., & Powles, D. L. (2012). Follow-up for improving psychological well being for women after a miscarriage (Review). Cochrane Database of Systematic Reviews, 3, CD008679. https://doi.org/10.1002/14651858.CD008679.pub2
Musters, A. M., Koot, Y. E. M., van den Boogaard, N. M., Kaaijk, E. M., Macklon, N. S., van der Veen, F., Nieuwkerk, P. T., & Goddijn, M. (2013). Supportive care for women with recurrent miscarriage: a survey to quantify women's preferences. Human Reproduction, 28(2), 398-405. https://doi.org/10.1093/humrep/des374
Nakano, Y., Akechi, T., Furukawa, T. A., & Sugiura-Ogasawara, M. (2013). Cognitive behavior therapy for psychological distress in patients with recurrent miscarriage. Psychology research and behavior management, 6, 37-43. https://doi.org/10.2147/PRBM.S44327
Nikčević, A. V., Kuczmierczyk, A. R., & Nicolaides, K. H. (2007). The influence of medical and psychological interventions on women's distress after miscarriage. Journal of psychosomatic research, 63(3), 283-290. https://doi.org/10.1016/j.jpsychores.2007.04.004
Palas Karaca, P., & Oskay, Ü. (2020). Effect of supportive care on the psychosocial health status of women who had a miscarriage. Perspectives in psychiatric care, 56(1), 69-77. https://doi.org/10.1111/ppc.12540
Rezaee, N., Afhami, H., & Navvabi-Rigi, S. (2024). The Effects of Positive Self-Talk on Anxiety and Grief Among Women with Spontaneous Abortion: A Quasi-Experimental Study. Shiraz E-Medical Journal, 25(3), e141769. https://doi.org/10.5812/semj-140347
Séjourné, N., Callahan, S., & Chabrol, H. (2010). The utility of a psychological intervention for coping with spontaneous abortion. Journal of Reproductive and Infant Psychology, 28(3), 287-296. https://doi.org/10.1080/02646830903487334
Séjourné, N., Callahan, S., & Chabrol, H. (2011). L'efficacité d'une brève intervention de soutien sur l'anxiété, la dépression, et le stress après une fausse couche. Journal de Gynécologie Obstétrique et Biologie de la Reproduction, 40(6), 530-536. https://doi.org/10.1016/j.jgyn.2011.01.015
Tavoli, Z., Mohammadi, M., Tavoli, A., Moini, A., Effatpanah, M., & Khedmat, L. (2018). Quality of life and psychological distress in women with recurrent miscarriage: a comparative study. Health and Quality of Life Outcomes, 16(1), 150. https://doi.org/10.1186/s12955-018-0982-z
Yeşildere Sağlam, H., Gursoy, E., & Kartal, Y. (2025). The effect of nursing care during pregnancy termination on women's prenatal grief, depression, anxiety, stress and coping levels: A randomized controlled study. Women & Health, 65(1), 50-65. https://doi.org/10.1080/03630242.2024.2441377
Zahmatkesh, M., Faal Siahkal, S., Alahverdi, F., Tahmasebi, G., & Ebrahimi, E. (2024). The role of art therapy on quality of life of women with recent pregnancy loss: A randomized clinical trial. PLoS One, 19(1), e0296464. https://doi.org/10.1371/journal.pone.0305403