Fear of Abandonment and Psychosomatic Symptoms: The Mediating Role of Attachment Insecurity
Keywords:
fear of abandonment, attachment insecurity, psychosomatic symptomsAbstract
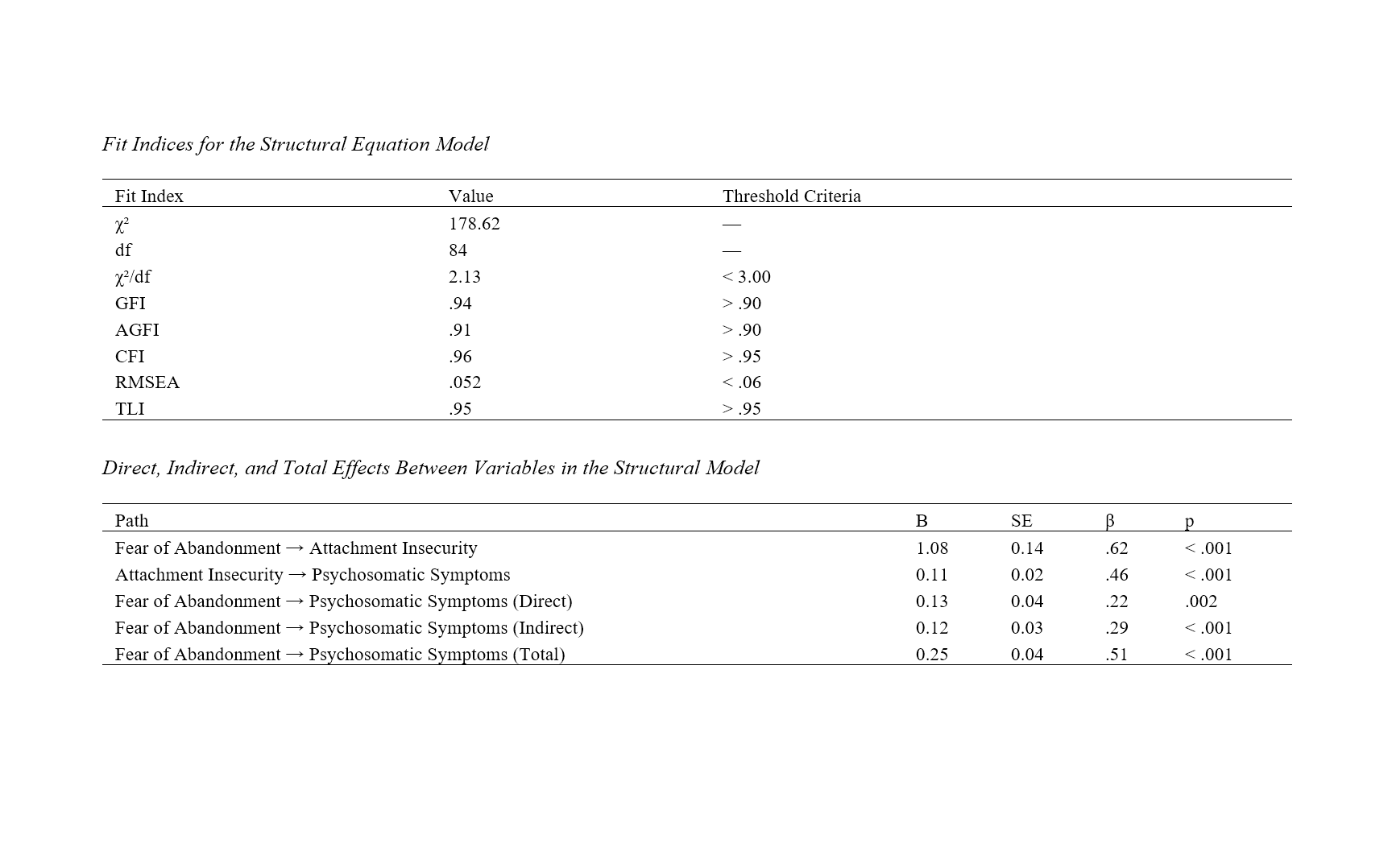
This study aimed to examine the relationship between fear of abandonment and psychosomatic symptoms and to investigate whether attachment insecurity mediates this relationship in a sample of Chinese young adults. The research followed a descriptive correlational design and included 419 participants from urban areas in China, selected based on the Morgan and Krejcie sampling table. Standardized instruments were used to measure fear of abandonment (Fear of Abandonment Scale), attachment insecurity (Experiences in Close Relationships–Revised), and psychosomatic symptoms (PHQ-15). Data were analyzed using Pearson correlation coefficients in SPSS-27 and structural equation modeling (SEM) in AMOS-21 to assess the mediating role of attachment insecurity. The results showed that fear of abandonment was positively correlated with both attachment insecurity (r = .62, p < .001) and psychosomatic symptoms (r = .51, p < .001). Attachment insecurity also had a significant positive correlation with psychosomatic symptoms (r = .57, p < .001). The structural model demonstrated good fit indices (χ²/df = 2.13, CFI = .96, RMSEA = .052), confirming the adequacy of the hypothesized model. Path analysis revealed that fear of abandonment significantly predicted attachment insecurity (β = .62, p < .001), which in turn predicted psychosomatic symptoms (β = .46, p < .001). The direct effect of fear of abandonment on psychosomatic symptoms remained significant (β = .22, p = .002), and the indirect effect through attachment insecurity was also significant (β = .29, p < .001), indicating partial mediation. These findings suggest that fear of abandonment contributes to psychosomatic symptoms both directly and indirectly through its impact on attachment insecurity. Addressing attachment-based vulnerabilities may be essential in the psychological treatment of individuals experiencing psychosomatic distress.
Downloads
References
Aeran, H., Singh, M., Singh, S., & Seth, J. (2024). Psychosomatic Disorders and Their Importance in Dentistry. International Journal of Oral Health Dentistry, 9(4), 242-246. https://doi.org/10.18231/j.ijohd.2023.046
Alsaffar, K. F. (2023). Overexcitability and Its Impact on Psychosomatic Disorders and the Role of "Cognitive Emotion Regulation" as a Mediating Variable. https://doi.org/10.21203/rs.3.rs-2397392/v1
Amirian, Z., Asadzadeh, H., & Mousavi, S. R. (2022). Prediction of Symptoms of Psychosomatic Disorders in University Students Based on Perfectionism Mediated by Smartphone Addiction. Caspian Journal of Health Research, 7(3), 151-158. https://doi.org/10.32598/cjhr.7.3.421.1.7
Bai, J. (2024). The Role of Insecure Attachment in Emotional Disorders: From Children to the Elderly. Lecture Notes in Education Psychology and Public Media, 51(1), 125-134. https://doi.org/10.54254/2753-7048/51/20240960
Chen, O., Guan, F., Zhan, C., & Li, Y. (2024). From Infected to Recovered: The Mediating Role of Sleep Quality Between Self-Compassion, Social Support and COVID-19 Psychosomatic Symptoms. BMC public health, 24(1). https://doi.org/10.1186/s12889-024-20657-9
Farahi, S., Naziri, G., Davodi, A., & Fath, N. (2023). The Mediating Role of Cognitive Emotion Regulation Strategies in the Relationship Between Early Maladaptive Schemas, Alexithymia, and Emotional Intelligence With Somatic Symptoms in People With Somatic Symptoms Disorder. Practice in Clinical Psychology, 11(3), 187-200. https://doi.org/10.32598/jpcp.11.3.887.1
Figueiredo‐Ferraz, H., Gil‐Monte, P. R., Grau‐Alberola, E., & Couto, B. R. D. (2021). The Mediator Role of Feelings of Guilt in the Process of Burnout and Psychosomatic Disorders: A Cross-Cultural Study. Frontiers in psychology, 12. https://doi.org/10.3389/fpsyg.2021.751211
Gao, L., Dahmen, A., Keller, F. M., Becker, P., & Lippke, S. (2021). The Mediation Effect of Phobic Anxiety on the Treatment Outcome of Activity and Participation Across Age: Comparison Between Online and Face-to-Face Rehabilitation Aftercare of an RCT. International journal of environmental research and public health, 18(20), 10919. https://doi.org/10.3390/ijerph182010919
Ghanavati, M. (2024). Comparing the Effectiveness of Emotion-Based and Attachment-Based Family Therapy on Emotional Distress Tolerance, Self-Differentiation and Alexithymia in Adolescent Girls With Psychosomatic Disorders. PDMD, 3(4), 139-152. https://doi.org/10.61838/kman.pdmd.3.4.10
Gil‐LaOrden, P., Carlotto, M. S., & Gil‐Monte, P. R. (2024). The Role of Guilt Feelings in the Development of the Burnout Process: The Influence on Psychosomatic Problems. Behavioral Sciences, 14(12), 1196. https://doi.org/10.3390/bs14121196
Habib, A., Ahmad, R., & Rehman, S. (2018). Prevalence of Associated Psychosomatic Symptoms in Patients of Irritable Bowel Syndrome. International Journal of Advances in Medicine, 5(6), 1515. https://doi.org/10.18203/2349-3933.ijam20184767
Habukawa, C., Nagamitsu, S., Koyanagi, K., Nishikii, Y., Yanagimoto, Y., Yoshida, S., Suzuki, Y., & Murakami, K. (2022). Early Intervention for Psychosomatic Symptoms of Adolescents in School Checkup. Pediatrics International. https://doi.org/10.1111/ped.15117
Jiao, X., Bai, R.-a., Li, N., & Liu, K. (2024). Influencing Factors on the Psychosomatic Health of Medical Staff Since the Normalized Stage of COVID-19 in Mainland China. European journal of public health, 34(3), 600-605. https://doi.org/10.1093/eurpub/ckae021
Kassel, J. D., Wardle, M., & Roberts, J. E. (2007). Adult attachment security and college student substance use. Addictive behaviors, 32(6), 1164-1176. https://doi.org/10.1016/j.addbeh.2006.08.005
Kealy, D., Rice, S. M., Chartier, G. B., & Cox, B. J. (2021). Investigating Attachment Insecurity and Somatosensory Amplification, and the Mediating Role of Interpersonal Problems. European Journal of Health Psychology, 28(3), 120-130. https://doi.org/10.1027/2512-8442/a000078
Medlej, B., & Greer, J. (2024). The Association Between Insecure Adult Attachment and Psychosomatic Symptoms as Mediated by Emotion Regulation. Nor Psy Bull, 1(1). https://doi.org/10.19164/npb.v1i1.1589
Narmetova, Y., Kuldosheva, G., & Bekmirov, T. (2021). The Psychological Services Role in the Psychodiagnostics and Psychocorrection of Psychosomatic Patients in the Psychoemotional Situation. International Journal of Multicultural and Multireligious Understanding, 8(12), 249. https://doi.org/10.18415/ijmmu.v8i12.3277
pardh, A. M., Karami, J., & Moradi, A. (2022). Role of Experiential Avoidance and Alexithymia in the Prediction of Psychosomatic Disorder Among the Employees at National Iranian South Oil Company. Journal of Ilam University of Medical Sciences, 30(2), 63-70. https://doi.org/10.52547/sjimu.30.2.63
Petelin, D. S., Kondrateva, K., Dzhibladze, T. A., & Volel, B. A. (2023). Psychosomatic Disorders Associated With Functional Diseases of the Female Reproductive System at Different Ages. Voprosy Ginekologii Akušerstva I Perinatologii, 22(5), 79-86. https://doi.org/10.20953/1726-1678-2023-5-79-86
Philippova, A., Malkina, O. L., Korotun, V. L., & Shatova, E. (2023). The Role of Somatic Factors in Early Childhood and Adolescent Psychosomatic Disorders. Bangladesh Journal of Medical Science, 22(3), 687-694. https://doi.org/10.3329/bjms.v22i3.66964
Pylypenko, N., Kovalova, O., Prokofieva, O., Kochkurova, O., Kriukova, M., & Zelinska, Y. (2022). Contemporary Approaches to Diagnosis, Psychotherapy and Neuro-Psychocorrection of Emotional Disorders in Psychosomatic Diseases. Brain Broad Research in Artificial Intelligence and Neuroscience, 13(1Sup1), 277-294. https://doi.org/10.18662/brain/13.1sup1/319
Pylypenko, N., Liasch, O., Chorna, I., Kompanovych, M., Levina, N., & Chystovska, Y. (2022). Neuropsychological Correction Technologies of Psychosomatic Disorders and Diseases. Brain Broad Research in Artificial Intelligence and Neuroscience, 13(2), 113-129. https://doi.org/10.18662/brain/13.2/335
Subbotina, R., Akopyan, A., Il’ina, I. Y., Ivashkina, M., & Bondaruk, E. (2022). Overcoming Strategies of Behavior of Women With Endometriosis. 69-77. https://doi.org/10.4018/978-1-6684-6299-7.ch006
Sumbaga, M., & Lapian, M. E. (2023). Attachment insecurity and marital satisfaction as a mediator to see the tendency of partner's infidelity.
Thornton, E. M., Dys, S. P., Hernandez, C. S., Smith, R. J., & Moretti, M. M. (2024). Parent–Youth Attachment Insecurity and Informant Discrepancies of Intrafamilial Aggression. Child Psychiatry & Human Development. https://doi.org/10.1007/s10578-023-01662-2
Werner, F. (2025). Psychosomatic - Psychotherapeutic Treatment of Stress-Related Disorders Impacts the Sphingolipid Metabolism Towards Increased Sphingosine and Sphingosine-1-Phosphate Levels. European Archives of Psychiatry and Clinical Neuroscience. https://doi.org/10.1007/s00406-025-01985-2
Downloads
Published
Submitted
Revised
Accepted
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.