Borderline Personality Features, Somatization, and Stress Reactivity: A Biopsychosocial Model
Keywords:
borderline personality features, somatization, stress reactivity, biopsychosocial model, personality pathologyAbstract
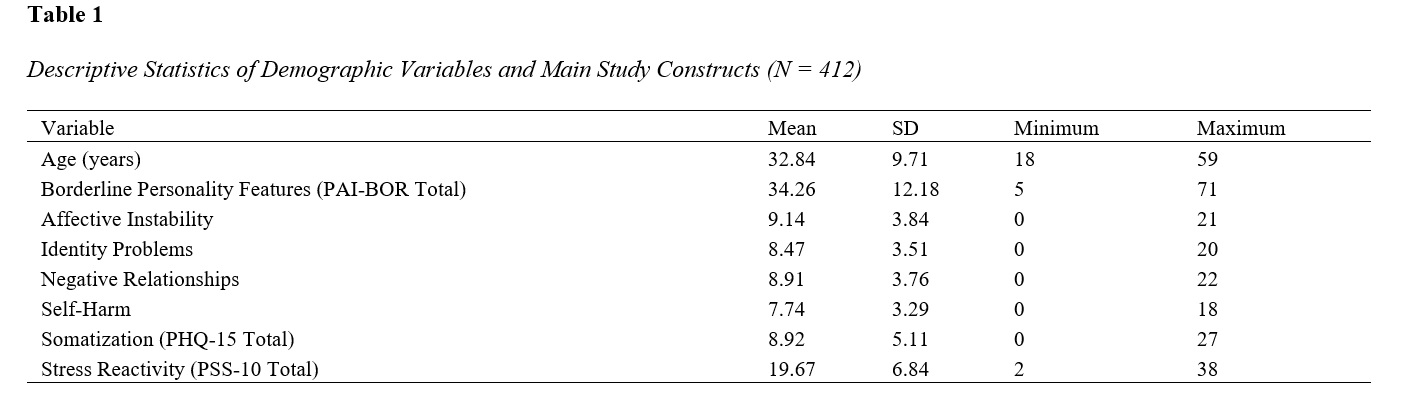
The objective of this study was to examine the relationships between borderline personality features, stress reactivity, and somatization within a biopsychosocial framework and to test the mediating role of stress reactivity in the association between borderline personality features and somatic symptom severity. This study used a cross-sectional correlational design and was conducted in an adult community sample from Colombia. Participants completed validated self-report measures assessing borderline personality features, perceived stress reactivity, and somatic symptoms. Borderline personality features were measured using the Borderline Features scale of the Personality Assessment Inventory, stress reactivity was assessed with the Perceived Stress Scale, and somatization was measured using the Patient Health Questionnaire–15. Data were analyzed using descriptive statistics, Pearson correlation analyses, multiple regression models, and regression-based mediation analyses with bootstrapped confidence intervals to test the proposed biopsychosocial model. Inferential analyses revealed significant positive correlations between borderline personality features and somatization, borderline personality features and stress reactivity, and stress reactivity and somatization. Multiple regression analysis indicated that both borderline personality features and stress reactivity independently and significantly predicted somatic symptom severity. Mediation analysis demonstrated that stress reactivity partially mediated the relationship between borderline personality features and somatization, with a significant indirect effect and a remaining significant direct effect of borderline personality features on somatic symptoms. The findings support an integrated biopsychosocial model in which borderline personality features are associated with increased somatic symptom burden both directly and indirectly through heightened stress reactivity, underscoring the central role of stress-related processes in the embodiment of personality-related emotional vulnerability.
Downloads
References
Allemand, M., Fend, H., & Hill, P. L. (2024). Negative Emotional Reactivity and Somatic Symptoms During Adolescence Predict Adult Health and Wellbeing in Early and Middle Adulthood. Journal of youth and adolescence, 53(7), 1513-1528. https://doi.org/10.1007/s10964-024-01940-9
Balaban, G., & Bilge, Y. (2025). Relationships Between Borderline Personality Disorder Traits and Emotional Reactivity and Reinforcement Sensitivity Systems: Network and Mediation Analysis. Psikiyatride Guncel Yaklasimlar - Current Approaches in Psychiatry, 17(Supplement 1), 314-330. https://doi.org/10.18863/pgy.1766719
Ballespí, S., Nonweiler, J., Sharp, C., Vives, J., & Barrantes‐Vidal, N. (2022). Self‐ but Not Other‐mentalizing Moderates the Association Between BPD Symptoms and Somatic Complaints in Community‐dwelling Adolescents. Psychology and Psychotherapy Theory Research and Practice, 95(4), 905-920. https://doi.org/10.1111/papt.12409
Bram, A. D. (2025). And/Or: Conditions to Differentiate From the Bipolar Spectrum or That Co-Occur. 105-127. https://doi.org/10.1037/0000430-010
Brud, P. P., & Cieciuch, J. (2024). Temperamental Underpinnings of Borderline Personality Disorder and Its Facets. Personality and Mental Health, 18(3), 205-215. https://doi.org/10.1002/pmh.1610
Deuter, C. E., Duesenberg, M., Hellmann‐Regen, J., Metz, S., Roepke, S., Wolf, O. T., Otte, C., & Wingenfeld, K. (2021). Psychosocial Stress Increases Testosterone in Patients With Borderline Personality Disorder, Post-Traumatic Stress Disorder and Healthy Participants. Borderline personality disorder and emotion dysregulation, 8(1). https://doi.org/10.1186/s40479-021-00145-x
Diiorio, C., Norton, S. A., Boudreaux, M. J., Chang, K., Michalski, L. J., Cruitt, P. J., Winstone, J. M. A., Oltmanns, T. F., & Bogdan, R. (2021). Borderline Personality Pathology, Health Behavior, and Inflammation: Potential Behavioral and Biological Mechanisms Underlying Childhood Physical Abuse and Age-Related Disease. https://doi.org/10.31234/osf.io/mg7ve
Ebrahimi, A., Taheri, E., Azamiyan, E., Naderi, Y., Samani, N. K., dehkordi, B. a., Soleimani, Z. A., & Dolatshahi, B. (2021). Borderline Personality Traits: The Roles of Childhood Teasing and Traumatic Experiences. Ajnpp, 11-16. https://doi.org/10.32592/ajnpp.2022.9.1.102
Engemann, L., Aweimer, A., Ewers, A., Afshari, F., Maiß, C., Kern, K., Lücke, T., Mügge, A., & Brüne, M. (2022). Altered Left Ventricular Myocardial Deformation in Young Women With Borderline Personality Disorder: An Echocardiographic Study. Psychosomatic Medicine, 84(5), 581-587. https://doi.org/10.1097/psy.0000000000001084
Farmanbar, F., Maredpour, A., & Malekzadeh, M. (2024). Effectiveness of Schema Therapy on Self-Differentiation and Rejection Sensitivity in Patients With Borderline Personality Disorder. Jayps, 5(2), 58-67. https://doi.org/10.61838/kman.jayps.5.2.7
García, C. Á., Navarro, L., Liétor, M. D. C. M., Iñiguez, I. C., & Giancola, A. S. (2021). The Overlap Between Complex Posttraumatic Stress Disorder and Borderline Personality Disorder. European Psychiatry, 64(S1), S754-S754. https://doi.org/10.1192/j.eurpsy.2021.1997
Kalimuthu, A. S. (2024). Simple Yogic Practices to Overcome All Psychiatric Disorders. Psychology and Mental Health Care, 8(7), 01-05. https://doi.org/10.31579/2637-8892/292
Kazemi, M., Amiri, H., Hosseini, S., & Chehri, A. (2024). Determining the Pattern of Relationship Between Sleep Disorder, Borderline Personality Disorder, and Post-Traumatic Stress Disorder in Nurses of Kermanshah City. PDMD, 3(3), 100-114. https://doi.org/10.61838/kman.pdmd.3.3.9
Mozo, E. H., Siegel, J. A., Jones, I. J., Rivera, D., & Blashill, A. J. (2025). The Association Between Minority Stressors, Intraminority Stressors, and Borderline Personality Disorder Symptomatology Among Sexual Minority Men. Personality Disorders Theory Research and Treatment, 16(2), 193-197. https://doi.org/10.1037/per0000705
Otto, B., Kokkelink, L., & Brüne, M. (2021). Borderline Personality Disorder in a “Life History Theory” Perspective: Evidence for a Fast “Pace-of-Life-Syndrome”. Frontiers in psychology, 12. https://doi.org/10.3389/fpsyg.2021.715153
Park, K. H. (2025). Borderline Personality Traits and Insomnia Severity: A Sequential Mediation Model of Maladaptive Cognitive Emotion Regulation Strategies and Pre-Sleep Arousal. Korean Journal of Stress Research, 33(4), 209-215. https://doi.org/10.17547/kjsr.2025.33.4.209
Ruffalo, M. L. (2025). On the Borderline Syndrome and Its Relationship to Schizophrenia. Psychodynamic Psychiatry, 53(2), 162-167. https://doi.org/10.1521/pdps.2025.53.2.162
Sahu, S., Chaudhury, S., Pathak, V., Singh, I., Mujawar, S., Arya, A., Mishra, A., Sharma, N., & Garg, G. (2021). Diverse Psychiatric Presentation Associated With Child Sexual Abuse. Industrial Psychiatry Journal, 30(Suppl 1), S221-S227. https://doi.org/10.4103/0972-6748.328866
Schittek, A., Roskam, I., & Mikolajczak, M. (2023). Parental Burnout and Borderline Personality Stand Out to Predict Child Maltreatment. Scientific reports, 13(1). https://doi.org/10.1038/s41598-023-39310-3
Schmaling, K. B., Fales, J., & Linehan, M. M. (2021). Treatment for Borderline Personality Disorder and Secondary Effects on Somatization. Journal of personality disorders, 35(4), 632-640. https://doi.org/10.1521/pedi_2020_34_469
St‐Amour, S., Cailhol, L., Lapointe, J., Ducasse, D., Landry, G., & Bernard, P. (2022). Pattern, Preferences, Barriers, and Correlates of Self-Reported Physical Activity in Adults With Borderline Personality Disorder: An Online Survey in Western Countries. https://doi.org/10.1101/2022.05.24.22275513
Vajawat, B., Venkataramu, N. V., Varshney, P., & Math, S. B. (2025). Somatization Disorders in Incarcerated Populations. 113-136. https://doi.org/10.1093/med/9780192858290.003.0009
Valdivieso-Jiménez, G., Pino-Zavaleta, D. A., Campos-Rodriguez, S. K., Ortiz-Saavedra, B., Fernández, M. F., & Benítes-Zapata, V. A. (2022). Efficacy and Safety of Aripiprazole in Borderline Personality Disorder: A Systematic Review. https://doi.org/10.21203/rs.3.rs-2292024/v1
Wardani, N. D., Widiastuti, M. I., Sudiyanto, A., Hardian, H., Lukman, P. R., Subagio, H. W., & Tugasworo, D. (2023). Clinical Practice Supportive Psychotherapy for Borderline Personality Disorder. Bali Medical Journal, 12(3), 2435-2439. https://doi.org/10.15562/bmj.v12i3.4614