AI-Based Profiling of Personality Disorder Traits Associated with Chronic Somatic Symptoms
Keywords:
chronic somatic symptoms, personality disorder traits, artificial intelligence, machine learning, psychosomatic medicineAbstract
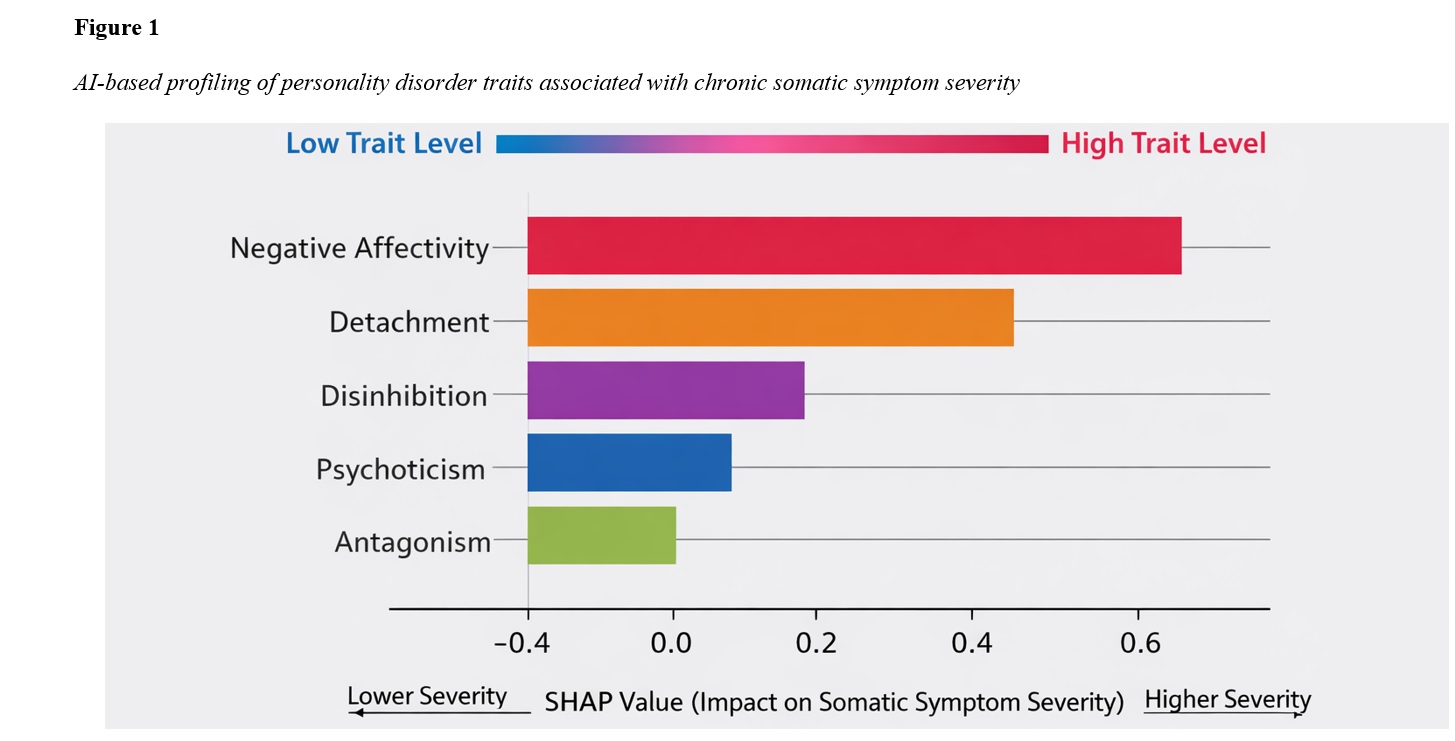
This study aimed to identify and model personality disorder–related trait profiles associated with the severity of chronic somatic symptoms using artificial intelligence–based analytical approaches. A cross-sectional observational design was employed with an adult sample recruited in Hungary. Participants completed standardized self-report measures assessing chronic somatic symptom severity, dimensional personality disorder traits, and psychological distress variables. Data were collected electronically following informed consent and ethical approval. Multiple supervised machine learning models, including regularized regression and ensemble-based algorithms, were trained to predict somatic symptom severity from personality trait dimensions while controlling for demographic and psychological covariates. Model performance was evaluated using cross-validation procedures, and explainable AI techniques were applied to determine the relative importance and direction of trait contributions. Ensemble machine learning models demonstrated superior predictive performance compared with linear approaches, indicating non-linear and interactive associations between personality traits and chronic somatic symptom severity. Negative affectivity emerged as the strongest predictor, followed by detachment, with both traits showing robust positive associations with symptom severity. Disinhibition and psychoticism contributed moderately, while antagonism exhibited a smaller but significant effect. Personality disorder traits provided substantial incremental explanatory value beyond anxiety and depressive symptoms, accounting for additional variance in somatic symptom severity. Explainability analyses confirmed the dominance of internalizing and emotion-related traits in the AI-derived personality profiles associated with higher symptom burden. The findings indicate that chronic somatic symptoms are strongly linked to specific configurations of maladaptive personality traits, particularly negative affectivity and detachment, and that AI-based modeling offers a powerful framework for capturing these complex relationships.
Downloads
References
Achenbach, J., Volkmann, L., Tran, A.-T., Jäger, B., Rhein, M., Glahn, A., Bernateck, M., & Karst, M. (2022). Neurohumoral Profiles and Childhood Adversity of Patients With Multisomatoform Disorder and Pain as the Leading Bodily Symptom. Disease Markers, 2022, 1-10. https://doi.org/10.1155/2022/7958375
Alsiri, N., Alhadhoud, M., Alkatefi, T., & Palmer, S. (2023). The Concomitant Diagnosis of Fibromyalgia and Connective Tissue Disorders: A Systematic Review. Seminars in Arthritis and Rheumatism, 58, 152127. https://doi.org/10.1016/j.semarthrit.2022.152127
Altuve, E. A., Rivera, M. A., & Crespi, C. A. (2022). Influence of COVID-19 in the Development of Delusional Ideas Disorder. A Case Report. European Psychiatry, 65(S1), S543-S544. https://doi.org/10.1192/j.eurpsy.2022.1391
Arévalo‐Martínez, A., Manso, J. M. M., Sánchez, M. E. G., Alonso, M. B., & Cordero, P. C. (2022). Psychopathological and Neuropsychological Disorders Associated With Chronic Primary Visceral Pain: Systematic Review. Frontiers in psychology, 13. https://doi.org/10.3389/fpsyg.2022.1031923
Bermpohl, F. M. g., & Martin, A. (2025). Efficacy of Cognitive Behavioral Therapy and Acceptance- And Mindfulness-Based Treatments in Adults With Bodily Distress: A Network Meta-Analysis. Psychotherapy and psychosomatics, 94(3), 207-224. https://doi.org/10.1159/000544825
Creed, F. (2023). Psychiatric Disorders Comorbid With General Medical Illnesses and Functional Somatic Disorders: The Lifelines Cohort Study. PLoS One, 18(5), e0286410. https://doi.org/10.1371/journal.pone.0286410
Doreste, A., Pujol, J., Penelo, E., Pérez, V., Blanco‐Hinojo, L., Martínez‐Vilavella, G., Ojeda, F., Monfort, J., & Deus, J. (2025). Personality Assessment Inventory in Fibromyalgia: Links to Functional, Physical–Somatic, and Emotional Impact. European Journal of Investigation in Health Psychology and Education, 15(8), 149. https://doi.org/10.3390/ejihpe15080149
Doreste, A., Pujol, J., Penelo, E., Pérez, V., Blanco‐Hinojo, L., Martínez‐Vilavella, G., Pardina-Torner, H., Ojeda, F., Monfort, J., & Deus, J. (2024). Exploring the Psychopathological Profile of Fibromyalgia: Insights From the Personality Assessment Inventory and Its Association With Disease Impact. Frontiers in psychology, 15. https://doi.org/10.3389/fpsyg.2024.1418644
Esteve, R., Bernardes, S. F., López‐Martínez, A. E., Martín‐Delgado, C. E., & Ramírez‐Maestre, C. (2021). The Informal Social Support for Autonomy and Dependence in Pain Inventory Spanish Version. Health & Social Care in the Community, 30(5). https://doi.org/10.1111/hsc.13632
García‐Domínguez, M. (2025). Fibromyalgia and Inflammation: Unrevealing the Connection. Cells, 14(4), 271. https://doi.org/10.3390/cells14040271
Gostoli, S., Ferrara, F., Quintavalle, L., Tommasino, S., Gigante, G., Montecchiarini, M., Urgese, A., Guolo, F., Subach, R., D’Oronzo, A., Polifemo, A., Buonfiglioli, F., Cennamo, V., & Rafanelli, C. (2024). Four-Year Follow-Up of Psychiatric and Psychosomatic Profile in Patients With Inflammatory Bowel Disease (IBD). BMC psychology, 12(1). https://doi.org/10.1186/s40359-024-01726-5
Guidi, J., Lucente, M., Sonino, N., & Fava, G. A. (2020). Allostatic Load and Its Impact on Health: A Systematic Review. Psychotherapy and psychosomatics, 90(1), 11-27. https://doi.org/10.1159/000510696
Hartmann, J., Bräscher, A. K., Forbush, K. T., Sellbom, M., Watson, D. G., & Witthöft, M. (2022). The Somatoform Spectrum Within the Hierarchical Taxonomy of Psychopathology System: A Taxometric Test of the Latent Structure. Psychosomatic Medicine, 84(9), 1067-1076. https://doi.org/10.1097/psy.0000000000001105
Islam, Z., D’Silva, A., Raman, M., & Nasser, Y. (2022). The Role of Mind Body Interventions in the Treatment of Irritable Bowel Syndrome and Fibromyalgia. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.1076763
Kachaner, A., Lemogne, C., Dave, J., Ranque, B., Broucker, T. d., & Meppiel, E. (2022). Somatic Symptom Disorder in Patients With Post-Covid-19 Neurological Symptoms: A Preliminary Report From the Somatic Study (Somatic Symptom Disorder Triggered by COVID-19). Journal of Neurology Neurosurgery & Psychiatry, 93(11), 1174-1180. https://doi.org/10.1136/jnnp-2021-327899
Kerber, A., Gewehr, E., Zimmermann, J., Sachser, C., Fegert, J. M., Knaevelsrud, C., & Spitzer, C. (2023). Adverse Childhood Experiences and Personality Functioning Interact Substantially in Predicting Depression, Anxiety, and Somatization. Personality and Mental Health, 17(3), 246-258. https://doi.org/10.1002/pmh.1578
Maria Ferreira de Almeida, M., Matos‐Pires, A., Simões, G., Gomes, A. I., & Coelho, A. (2025). The Battle With Cancer When You Have a Personality Disorder. European Psychiatry, 68(S1), S949-S949. https://doi.org/10.1192/j.eurpsy.2025.1925
Meade, E., & Garvey, M. (2022). The Role of Neuro-Immune Interaction in Chronic Pain Conditions; Functional Somatic Syndrome, Neurogenic Inflammation, and Peripheral Neuropathy. International Journal of Molecular Sciences, 23(15), 8574. https://doi.org/10.3390/ijms23158574
Meulen, W. G. t., Draisma, S., Hemert, A. M. v., Schoevers, R. A., Kupka, R., Beekman, A. T., & Penninx, B. W. (2021). Depressive and Anxiety Disorders in Concert–A Synthesis of Findings on Comorbidity in the NESDA Study. Journal of affective disorders, 284, 85-97. https://doi.org/10.1016/j.jad.2021.02.004
Noviello, D., Costantino, A., Muscatello, A., Bandera, A., Consonni, D., Vecchi, M., & Basilisco, G. (2021). Functional Gastrointestinal and Somatoform Symptoms Five Months After SARS‐CoV‐2 Infection: A Controlled Cohort Study. Neurogastroenterology & Motility, 34(2). https://doi.org/10.1111/nmo.14187
Ohse, L., Zimmermann, J., Kerber, A., Kampe, L., Mohr, J., Kendlbacher, J., Busch, O., Rentrop, M., & Hörz‐Sagstetter, S. (2023). Reliability, Structure, and Validity of Module I (Personality Functioning) of the Structured Clinical Interview for the Alternative DSM–5 Model for Personality Disorders (SCID-5-AMPD-I). Personality Disorders Theory Research and Treatment, 14(3), 287-299. https://doi.org/10.1037/per0000576
Onofrj, M., Rosa, M. A. D., Russo, M., Ajdinaj, P., Calisi, D., Thomas, A., & Sensi, S. L. (2024). Psychiatric Disorders and Cognitive Fluctuations in Parkinson’s Disease: Changing Approaches in the First Decades of the 21st Century. Brain Sciences, 14(12), 1233. https://doi.org/10.3390/brainsci14121233
Orzechowska, A., Maruszewska, P., Gałecka, M., Hyland, P., Boduszek, D., Gałecki, P., & Bliźniewska-Kowalska, K. (2023). Emotional Control in Selected Somatic and Psychiatric Diseases. BMC psychiatry, 23(1). https://doi.org/10.1186/s12888-023-05321-7
Rometsch, C., Mansueto, G., Bermpohl, F. M. g., Martin, A., & Cosci, F. (2024). Prevalence of Functional Disorders Across Europe: A Systematic Review and Meta-Analysis. European Journal of Epidemiology, 39(6), 571-586. https://doi.org/10.1007/s10654-024-01109-5
Rometsch, C., Martin, A., & Cosci, F. (2025). Predictors of Treatment Success of Psychotherapy in Functional Disorders: A Systematic Review of the Literature. Clinical Psychology & Psychotherapy, 32(2). https://doi.org/10.1002/cpp.70075
Schrottenberg, V. v., Kerber, A., Sterner, P., Teusen, C., Beigel, P., Linde, K., Henningsen, P., Herpertz, S. C., Gensichen, J., & Schneider, A. (2024). Exploring Associations of Somatic Symptom Disorder With Personality Dysfunction and Specific Maladaptive Traits. Psychopathology, 1-12. https://doi.org/10.1159/000540161
Siracusa, R., Paola, R. D., Cuzzocrea, S., & Impellizzeri, D. (2021). Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. International Journal of Molecular Sciences, 22(8), 3891. https://doi.org/10.3390/ijms22083891
Ulual, P., Özer, V., Uyar, M., Alataş, İ., Özpınar, G., & Güçlü, O. (2023). The Relationship Between Somatization and Depression and Anxiety Levels of Parents With Children Diagnosed With Spina Bifida. European Psychiatry, 66(S1), S587-S587. https://doi.org/10.1192/j.eurpsy.2023.1227
Романов, Д. В., Nasonova, T. I., Исайкин, А. И., Filileeva, O. V., Sheyanov, A. M., Iuzbashian, P. G., Voronova, E. I., & Парфенов, В. А. (2023). Personality Disorders and Traits of ABC Clusters in Fibromyalgia in a Neurological Setting. Biomedicines, 11(12), 3162. https://doi.org/10.3390/biomedicines11123162