Predicting Somatic Symptom Disorder Using Ensemble Learning on Personality, Stress, and Emotion Regulation Data
Keywords:
Somatic symptom disorder, ensemble learning, personality traits, perceived stress, emotion regulation, machine learningAbstract
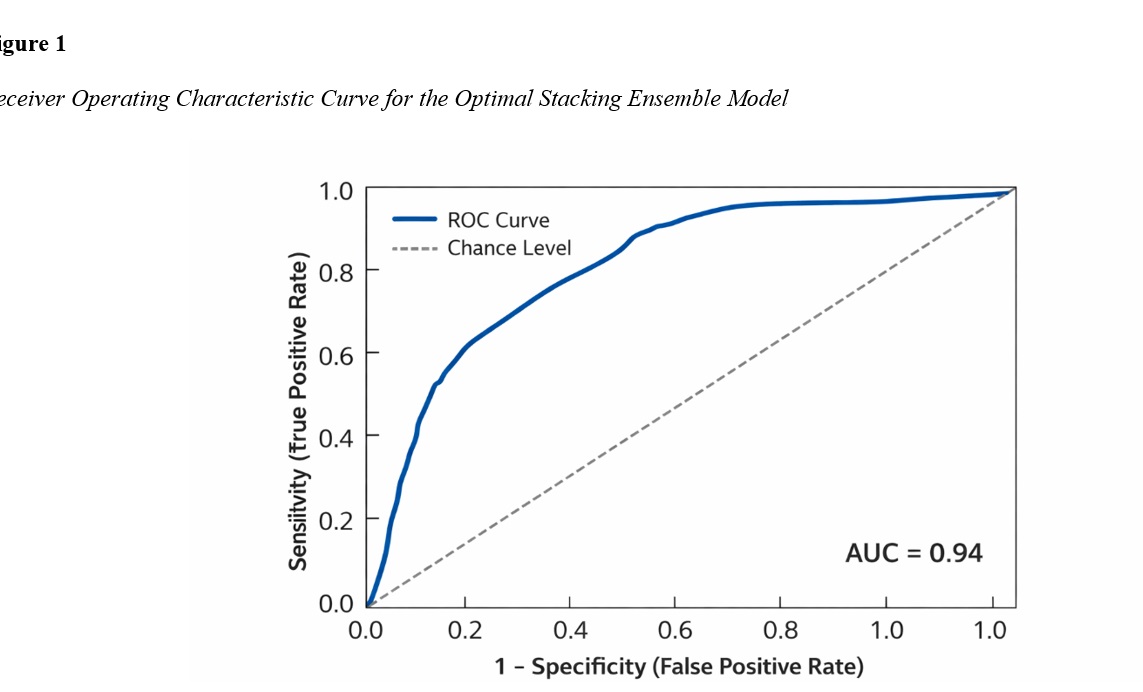
The objective of this study was to develop and evaluate ensemble learning models to predict somatic symptom disorder based on personality traits, perceived stress, and emotion regulation variables. This cross-sectional study was conducted on an adult sample from South Africa using a predictive modeling design. Participants completed standardized self-report measures assessing somatic symptom severity, personality traits, perceived stress, and multiple dimensions of emotion regulation. Data preprocessing included handling missing values, standardization of continuous variables, and feature preparation for machine learning analysis. Several base classifiers were trained and integrated using ensemble learning techniques, including random forest, gradient boosting, and stacking. Model training and evaluation were performed using stratified k-fold cross-validation to ensure robustness and reduce overfitting. Predictive performance was assessed using multiple inferential metrics, including accuracy, sensitivity, specificity, precision, F1-score, and area under the receiver operating characteristic curve (AUC). Feature importance and incremental modeling analyses were conducted to examine the relative and combined contributions of predictor domains. The ensemble learning models demonstrated strong predictive performance, with the stacking ensemble yielding the highest accuracy and AUC, indicating excellent discrimination between higher and lower somatic symptom severity. Neuroticism and perceived stress emerged as the most influential predictors, followed by key emotion regulation difficulties, particularly impulse control problems and limited access to adaptive regulation strategies. Incremental analyses showed that models incorporating personality traits alone achieved moderate prediction, which significantly improved with the addition of perceived stress and further improved when emotion regulation variables were included.
Downloads
References
Bablis, P., Day, R. R., Bablis, S. R., & Pollard, H. (2025). Neuro Emotional Technique as a Treatment for Separation Anxiety Related to Prenatal Stress: A Case Report. Cureus. https://doi.org/10.7759/cureus.83558
Brown, R. L., Chen, M. A., Paoletti, J., Dicker, E. E., Wu‐Chung, E. L., LeRoy, A. S., Majd, M., Suchting, R., Thayer, J. F., & Fagundes, C. P. (2022). Emotion Regulation, Parasympathetic Function, and Psychological Well-Being. Frontiers in psychology, 13. https://doi.org/10.3389/fpsyg.2022.879166
Carmassi, C., Conti, L., Gravina, D., Nardi, B., & Dell’Osso, L. (2022). Emotional Dysregulation as Trans-Nosographic Psychopathological Dimension in Adulthood: A Systematic Review. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.900277
Conti, L., Fantasia, S., Violi, M., Dell’Oste, V., Pedrinelli, V., & Carmassi, C. (2023). Emotional Dysregulation and Post-Traumatic Stress Symptoms: Which Interaction in Adolescents and Young Adults? A Systematic Review. Brain Sciences, 13(12), 1730. https://doi.org/10.3390/brainsci13121730
Everaert, J., Benisty, H., Polack, R. G., Joormann, J., & Mishne, G. (2022). Which Features of Repetitive Negative Thinking and Positive Reappraisal Predict Depression? An in-Depth Investigation Using Artificial Neural Networks With Feature Selection. Journal of Psychopathology and Clinical Science, 131(7), 754-768. https://doi.org/10.1037/abn0000775
Gatta, M., Angelico, C., Rigoni, F., Raffagnato, A., & Miscioscia, M. (2022). Alexithymia and Psychopathological Manifestations Centered on the Body: Somatization and Self-Harm. Journal of clinical medicine, 11(8), 2220. https://doi.org/10.3390/jcm11082220
Hornstein, L., Schleicher, D., Ecker, A., Kandsperger, S., Brunner, R., & Jarvers, I. (2025). Dark Triad Traits, Alexithymia, and Emotion Regulation as Predictors of Depression, Anxiety, and Stress in Clinical and Non-Clinical Samples. Frontiers in psychology, 16. https://doi.org/10.3389/fpsyg.2025.1674630
Ilen, L., Feller, C., & Schneider, M. (2023). Cognitive Emotion Regulation Difficulties Increase Affective Reactivity to Daily-Life Stress in Autistic Adolescents and Young Adults. Autism, 28(7), 1703-1718. https://doi.org/10.1177/13623613231204829
Impis, O., Zartaloudi, A., Grapsa, E., & Gerogianni, G. (2025). Association Between Emotional Intelligence and Stress Management in Hemodialysis Patients. Clinics and Practice, 15(8), 153. https://doi.org/10.3390/clinpract15080153
Janiri, D., Moccia, L., Dattoli, L., Pepe, M., Molinaro, M., Martin, V. D., Chieffo, D., Nicola, M. D., Fiorillo, A., Janiri, L., & Sani, G. (2021). Emotional Dysregulation Mediates the Impact of Childhood Trauma on Psychological Distress: First Italian Data During the Early Phase of COVID-19 Outbreak. Australian & New Zealand Journal of Psychiatry, 55(11), 1071-1078. https://doi.org/10.1177/0004867421998802
Janiri, D., Petracca, M., Moccia, L., Solito, M., Monaco, M. R. L., Cerbarano, M. L., Piano, C., Imbimbo, I., Nicola, M. D., Simonetti, A., Sani, G., & Bentivoglio, A. R. (2023). Functional Movement Disorders During COVID-19: Psychological Distress, Affective Temperament and Emotional Dysregulation. Journal of Personalized Medicine, 13(2), 175. https://doi.org/10.3390/jpm13020175
Kebets, V., Favre, P., Houenou, J., Polosan, M., Perroud, N., Aubry, J. M., Ville, D. V. D., & Piguet, C. (2021). Fronto-Limbic Neural Variability as a Transdiagnostic Correlate of Emotion Dysregulation. Translational psychiatry, 11(1). https://doi.org/10.1038/s41398-021-01666-3
Lilliengren, P., Mechler, J., Lindqvist, K., Maroti, D., & Johansson, R. (2025). The Efficacy of Experiential Dynamic Therapies: A 10‐Year Systematic Review and Meta‐Analysis Update. Clinical Psychology & Psychotherapy, 32(3). https://doi.org/10.1002/cpp.70086
Lopes, A. R., & Nihei, O. K. (2021). Depression, Anxiety and Stress Symptoms in Brazilian University Students During the COVID-19 Pandemic: Predictors and Association With Life Satisfaction, Psychological Well-Being and Coping Strategies. PLoS One, 16(10), e0258493. https://doi.org/10.1371/journal.pone.0258493
Meherali, S., Punjani, N. S., Louie‐Poon, S., Rahim, K. A., Das, J. K., Salam, R. A., & Lassi, Z. S. (2021). Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. International journal of environmental research and public health, 18(7), 3432. https://doi.org/10.3390/ijerph18073432
Pedrini, L., Meloni, S., Lanfredi, M., Ferrari, C., Geviti, A., Cattaneo, A., & Rossi, R. (2022). Adolescents’ Mental Health and Maladaptive Behaviors Before the Covid-19 Pandemic and 1-Year After: Analysis of Trajectories Over Time and Associated Factors. Child and adolescent psychiatry and mental health, 16(1). https://doi.org/10.1186/s13034-022-00474-x
Piguet, C., Celen, Z., Meuleman, B., Schilliger, Z., Smith, M. M., Mendola, E., Pham, E., Jouabli, S., Ivanova, V., Murray, R. J., Klauser, P., & Merglen, A. (2025). Impact of a Mindfulness‐Based Intervention on Symptoms and Emotion Regulation Strategies in Young Adolescents From the General Population: A Randomized Controlled Trial. Depression and Anxiety, 2025(1). https://doi.org/10.1155/da/2679049
Renzi, A., Conte, G., & Tambelli, R. (2022). Somatic, Emotional and Behavioral Symptomatology in Children During COVID-19 Pandemic: The Role of Children’s and Parents’ Alexithymia. Healthcare, 10(11), 2171. https://doi.org/10.3390/healthcare10112171
Sampedro, F., Aracil‐Bolaños, I., Farrés, C. C. i., Soler, J., Schmidt, C., Elices, M., Pomarol‐Clotet, E., Salvador, R., Vega, D., & Pascual, J. C. (2021). A Functional Connectivity Study to Investigate the Role of the Right Anterior Insula in Modulating Emotional Dysfunction in Borderline Personality Disorder. Psychosomatic Medicine, 84(1), 64-73. https://doi.org/10.1097/psy.0000000000001019
Schmitz, M., Back, S. N., Seitz, K., Harbrecht, N. K., Streckert, L., Schulz, A., Herpertz, S. C., & Bertsch, K. (2023). The Impact of Traumatic Childhood Experiences on Interoception: Disregarding One’s Own Body. Borderline personality disorder and emotion dysregulation, 10(1). https://doi.org/10.1186/s40479-023-00212-5
Schneider, I., Herpertz, S. C., Ueltzhöffer, K., & Neukel, C. (2023). Stress and Reward in the Maternal Brain of Mothers With Borderline Personality Disorder: A Script-Based fMRI Study. European Archives of Psychiatry and Clinical Neuroscience, 274(1), 117-127. https://doi.org/10.1007/s00406-023-01634-6
Shahane, A. D., Godfrey, D. A., & Denny, B. T. (2023). Predicting Real-World Emotion and Health From Spontaneously Assessed Linguistic Distancing Using Novel Scalable Technology. Emotion, 23(7), 2002-2012. https://doi.org/10.1037/emo0001211
Sheikh, W. G. E., Abou‐Abbass, H., Bizri, M., Tamim, H., Karout, L., Allouch, F., Chehade, R., Ghannam, M., Fares, Y., Nasser, Z., Al‐Hajj, S., Harati, H., & Kobeissy, F. (2025). The Impact of Posttraumatic Stress Disorder and Head Injury on Reactive and Appetitive Aggression in Adult Syrian Refugees in Lebanon. Psychological Trauma Theory Research Practice and Policy, 17(1), 67-76. https://doi.org/10.1037/tra0001796
Silva, D. C. d., Rabelo-da-Ponte, F. D., Salati, L. R., & Lobato, M. I. R. (2022). Heterogeneity in Gender Dysphoria in a Brazilian Sample Awaiting Gender-Affirming Surgery: A Data-Driven Analysis. BMC psychiatry, 22(1). https://doi.org/10.1186/s12888-022-03727-3
Ucuz, I., Çiçek, A. U., Celik, M. K., Akan, M., Kesriklioglu, E., Güngör, S., & Özcan, Ö. (2023). Emotional Dysregulation and Temperament-Character Traits in Adolescents With Functional Neurological Symptom Disorder (Conversion Disorder). The Journal of Nervous and Mental Disease, 212(3), 152-158. https://doi.org/10.1097/nmd.0000000000001746
Wei, M., Li, J., Wang, X., Su, Z., & Luo, Y. L. L. (2024). Will the Dark Triad Engender Psychopathological Symptoms or Vice Versa? A Three‐Wave Random Intercept Cross‐Lagged Panel Analysis. Journal of personality, 93(3), 767-780. https://doi.org/10.1111/jopy.12974
Yaroslavsky, I., Bush, A. H., & France, C. M. (2020). Emotion Regulation Deficits Mediate Childhood Sexual Abuse Effects on Stress Sensitization and Depression Outcomes. Development and Psychopathology, 34(1), 157-170. https://doi.org/10.1017/s095457942000098x
Zwir, I., Arnedo, J., Mesa, A., Val, C. d., Erausquin, G. A. d., & Cloninger, C. R. (2023). Temperament &Amp; Character Account for Brain Functional Connectivity at Rest: A Diathesis-Stress Model of Functional Dysregulation in Psychosis. Molecular Psychiatry, 28(6), 2238-2253. https://doi.org/10.1038/s41380-023-02039-6