Emotional and Cognitive Effects of Long-Term Antipsychotic Medication Use: A Qualitative Study
Keywords:
Antipsychotic medication, long-term use, emotional effects, cognitive effects, schizophrenia, mental health, patient experiencesAbstract
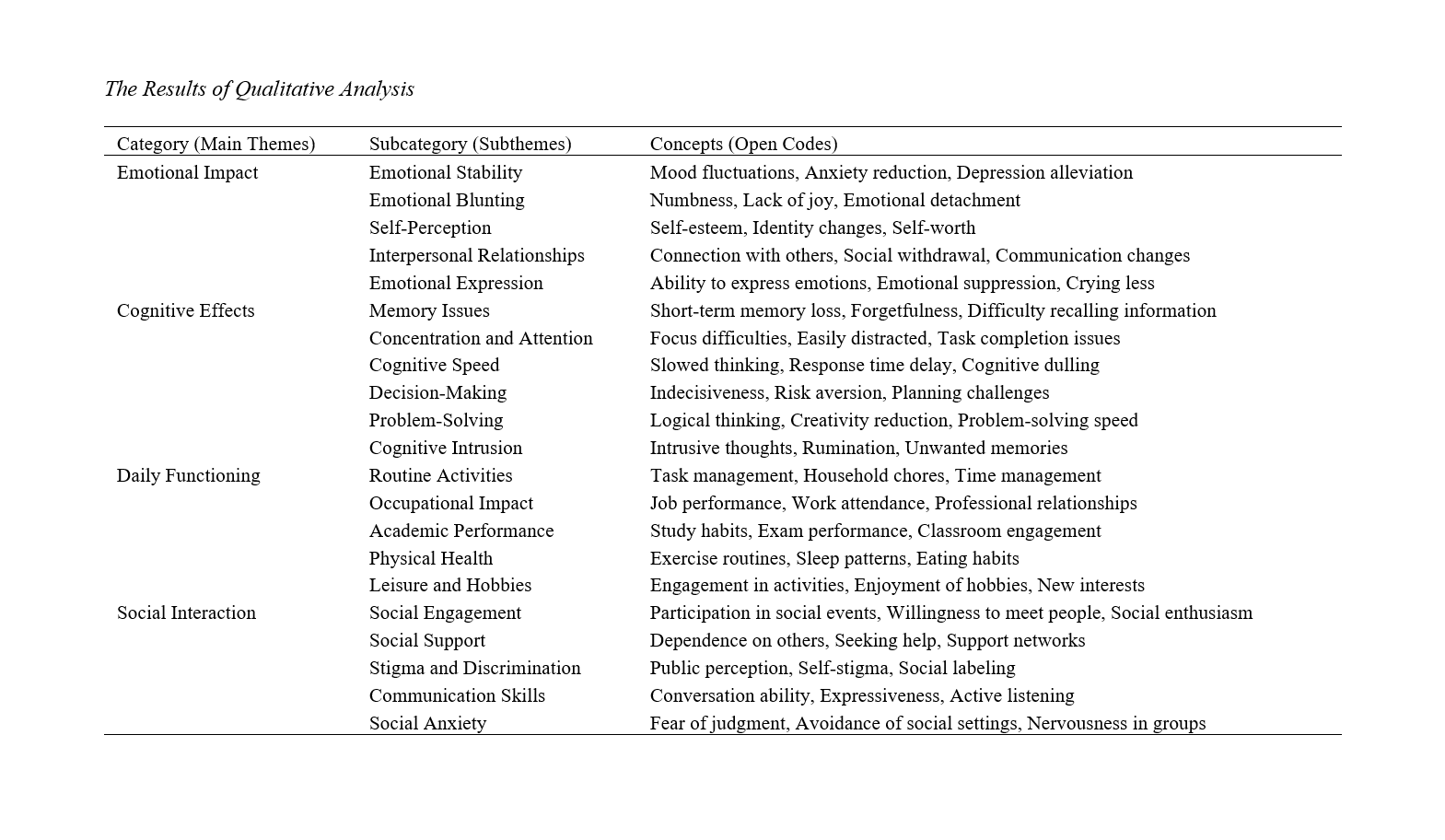
This study aimed to explore the emotional and cognitive effects of long-term antipsychotic medication use. By understanding these impacts, the study seeks to provide a comprehensive view of the lived experiences of individuals who have been on antipsychotic medications for extended periods, highlighting both the benefits and the potential challenges. A qualitative research design was employed using a phenomenological approach to capture in-depth personal experiences. A purposive sampling method recruited 26 participants who had been on antipsychotic medications for at least five years. Data were collected through semi-structured interviews, which were transcribed verbatim and analyzed using thematic analysis to identify common themes and patterns in the participants' experiences. The study achieved theoretical saturation, ensuring that no new themes emerged from the data. The analysis revealed four main themes: emotional impact, cognitive effects, daily functioning, and social interaction. Participants reported significant emotional blunting, including reduced pleasure and emotional responsiveness, alongside cognitive impairments such as memory deficits and diminished attention span. Challenges in daily functioning, such as difficulties in managing routine activities and occupational tasks, were prominent. Social interactions were also affected, with participants experiencing reduced social engagement, dependency on support networks, and stigma related to medication use. These findings are consistent with previous studies, underscoring the profound impact of long-term antipsychotic use on various aspects of life. Long-term use of antipsychotic medications, while essential for managing severe psychiatric conditions, is associated with significant emotional and cognitive side effects that impact patients' quality of life. Healthcare providers should be aware of these effects and engage in regular assessments and open communication with patients to address and mitigate these challenges. Personalized treatment approaches, psychoeducation, and support groups can enhance patients' well-being and treatment adherence.
Downloads
References
Citrome, L., Belcher, E., Stacy, S., Suett, M., Mychaskiw, M. A., & Salinas, G. D. (2022). Management of Schizophrenia With Long-Acting Injectable Antipsychotic Medications: An Assessment of the Educational Needs of Clinicians. Neuropsychiatric Disease and Treatment, Volume 18, 111-123. https://doi.org/10.2147/ndt.s326299
Crellin, N., Priebe, S., Morant, N., Lewis, G., Freemantle, N., Horne, R., Pinfold, V., Kent, L., Smith, R., Darton, K., Cooper, R., Long, M., Thompson, J., Gruenwald, L., Freudenthal, R., & Stansfeld, J. (2022). An Analysis of Views About Supported Reduction or Discontinuation of Antipsychotic Treatment Among People With Schizophrenia and Other Psychotic Disorders. BMC psychiatry, 22(1).https://doi.org/10.1186/s12888-022-03822-5
Desmarais, J. E., & Margolese, H. C. (2012). Anticholinergics in the Era of Atypical Antipsychotics: Short-Term or Long-Term Treatment? Journal of Psychopharmacology, 26(9), 1167-1174.https://doi.org/10.1177/0269881112447988
Goetz, C. G., Fan, W., & Leurgans, S. E. (2008). Antipsychotic Medication Treatment for Mild Hallucinations in Parkinson's Disease: Positive Impact on Long‐term Worsening. Movement Disorders, 23(11), 1541-1545.https://doi.org/10.1002/mds.22132
Hartung, D., Wisdom, J. P., Pollack, D. A., Hamer, A. M., Haxby, D. G., Middleton, L., & McFarland, B. H. (2008). Patterns of Atypical Antipsychotic Subtherapeutic Dosing Among Oregon Medicaid Patients. The Journal of Clinical Psychiatry,69(10), 1540-1547.https://doi.org/10.4088/jcp.v69n1003
Jaworska, N., Moss, S. J., Krewulak, K. D., Stelfox, Z., Niven, D. J., Ismail, Z., Burry, L., & Fiest, K. M. (2022). Antipsychotic Prescribing Practices and Patient, Family Member and Healthcare Professional Perceptions of Antipsychotic Prescribing in Acute Care Settings: A Scoping Review Protocol. BMJ open, 12(6), e057585.https://doi.org/10.1136/bmjopen-2021-057585
Mittal, S., Prasad, S., & Ghosh, A. (2017). Antipsychotic-Induced Hyperprolactinaemia: Case Studies and Review. Postgraduate Medical Journal, 94(1110), 226-229.https://doi.org/10.1136/postgradmedj-2017-135221
Murray, R. M., Quattrone, D., Natesan, S., Os, J. v., Nordentoft, M., Howes, O., Forti, M. D., & Taylor, D. (2016). Should Psychiatrists Be More Cautious About the Long-Term Prophylactic Use of Antipsychotics? The British Journal of Psychiatry, 209(5), 361-365.https://doi.org/10.1192/bjp.bp.116.182683
Price, R., Salavati, B., Graff-Guerrero, A., Blumberger, D. M., Mulsant, B. H., Daskalakis, Z. J., & Rajji, T. K. (2014). Effects of Antipsychotic D2 Antagonists on Long-Term Potentiation in Animals and Implications for Human Studies. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 54, 83-91.https://doi.org/10.1016/j.pnpbp.2014.05.001
Revel, F. G., Moreau, J. L., Pouzet, B., Mory, R., Bradaı̈ a, A., Buchy, D., Metzler, V., Chaboz, S., Zbinden, K. G., Galley, G., Norcross, R. D., Tuerck, D., Bruns, A., Morairty, S. R., Kilduff, T. S., Wallace, T. L., Risterucci, C., Wettstein, J. G., & Hoener, M. C. (2012). A New Perspective for Schizophrenia: TAAR1 Agonists Reveal Antipsychotic- And Antidepressant-Like Activity, Improve Cognition and Control Body Weight. Molecular Psychiatry, 18(5), 543-556.https://doi.org/10.1038/mp.2012.57
Sohler, N., Barnes, D. M., Cohen, G. H., Prins, S. J., & Schwartz, S. (2016). Weighing the Evidence for Harm From Long-Term Treatment With Antipsychotic Medications: A Systematic Review. American Journal of Orthopsychiatry, 86(5), 477-485.https://doi.org/10.1037/ort0000106
Townsend, M. J., Pareja, K., Buchanan-Hughes, A., Worthington, E., Piccoli, D. A., Brubaker, M., Houle, C. R., Mose, T. N., & Waters, H. C (2022). Antipsychotic-Related Stigma and the Impact on Treatment Choices: A Systematic Review and Framework Synthesis. Patient Preference and Adherence, Volume 16, 373-401.https://doi.org/10.2147/ppa.s343211
Wink, L., Pedapati, E. V., Horn, P. S., McDougle, C. J., & Erickson, C. A. (2017). Multiple Antipsychotic Medication Use in Autism Spectrum Disorder. Journal of Child and Adolescent Psychopharmacology, 27(1), 91-94.https://doi.org/10.1089/cap.2015.0123
Downloads
Additional Files
Published
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.