Comparison of the Effectiveness of Eye Movement Desensitization and Reprocessing and Mindfulness-Based Cognitive Therapy on Working Memory in Individuals with Primary Insomnia
Keywords:
Eye Movement Desensitization and Reprocessing (EMDR), Mindfulness-Based Cognitive Therapy (MBCT), working memory, primary insomniaAbstract
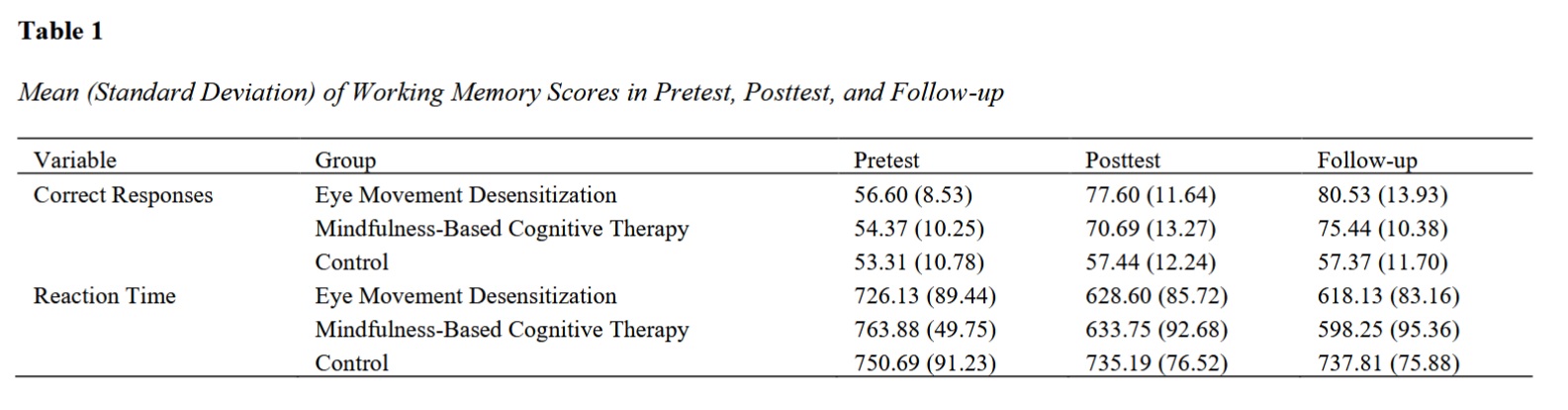
Primary insomnia is one of the common disorders that has a significant negative impact on cognitive functioning, including working memory. The aim of the present study was to compare the effectiveness of Eye Movement Desensitization and Reprocessing (EMDR) and Mindfulness-Based Cognitive Therapy (MBCT) on working memory in individuals with primary insomnia. A total of 48 participants (16 in each group) were selected from among individuals with primary insomnia through convenience sampling while observing the inclusion criteria. They were then randomly assigned to two experimental groups and one control group. The research design was a quasi-experimental pretest–posttest design with a one-month follow-up. The data collection instrument was the N-Back Test (1958). Mixed ANOVA, Bonferroni post hoc test, and SPSS (Version 26) were used for data analysis. The results indicated that both Eye Movement Desensitization and Reprocessing and Mindfulness-Based Cognitive Therapy were effective in improving working memory in individuals with primary insomnia; however, there was no significant difference between the effectiveness of the two treatments. The findings of this study showed that both therapeutic approaches were effective in improving working memory. Nevertheless, future studies with larger sample sizes and long-term follow-ups are required to examine the stability of treatment effects and enhance the generalizability of the results.
Downloads
References
American Psychiatric, A. (2013). Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596
Baddeley, A. (2003). Working memory and language: An overview. Journal of Communication Disorders, 36(3), 189–208. https://doi.org/10.1016/S0021-9924(03)00019-4
Ballesio, A., Aquino, M. R., Kyle, S. D., Ferlazzo, F., & Lombardo, C. (2019). Executive functions in insomnia disorder: a systematic review and exploratory meta-analysis. Frontiers in psychology, 10, 101. https://doi.org/10.3389/fpsyg.2019.00101
Behnam-Moghadam, A., Mahmoudi, A., Mardpour, A., Zadeh-Bagheri, F., & Behnam-Moghadam, M. (2024). Examining the effect of EMDR on enhancing working memory in patients with myocardial infarction: A randomized clinical trial. Journal of Disability Studies, 14, 48–48.
Behnam-Moghadam, A., Mardpour, A., Zadeh-Bagheri, F., & Mahmoudi, A. (2023). Investigating the effect of eye movement desensitization and reprocessing (EMDR) on cognitive performance in patients with myocardial infarction. Armaghan-e-Danesh, 28(4), 442–454. https://doi.org/10.61186/armaghanj.28.4.442
Besak-Nejad, S., Aghajani-Afjedi, A., & Zargar, Y. (2011). Investigating the effectiveness of mindfulness-based cognitive therapy on sleep quality and quality of life in female university students. Psychological Achievements, 18(2), 181–198. https://psychac.scu.ac.ir/article_11726.html
Çeliköz, N., Erisen, Y., & Sahin, M. (2019). Cognitive learning theories with emphasis on latent learning, gestalt and information processing theories. Journal of educational and instructional studies in the world, 9(3). https://eric.ed.gov/?id=ED598366
Chen, J., Wang, Z., & Wu, S. (2025). Comparison of the effects of verbal and visuospatial working memory training on reading comprehension of students with special needs. International Journal of Developmental Disabilities, 1–12. https://doi.org/10.1080/20473869.2025.2473405
De Zambotti, M., Covassin, N., De Min Tona, G., Sarlo, M., & Stegagno, L. (2011). Sleep onset and cardiovascular activity in primary insomnia. Journal of Sleep Research, 20(2), 318–325. https://doi.org/10.1111/j.1365-2869.2010.00871.x
Ding, C., Fan, J., Yuan, F., Feng, G., Gong, W., Song, C., Ma, Y., Chen, Z., & Liu, A. (2022). Association between physical activity, sedentary behaviors, sleep, diet, and adiposity among children and adolescents in China. Obesity Facts, 15(1), 26–35. https://doi.org/10.1159/000519268
Gielkens, E. M., Rossi, G., van Alphen, S. P., & Sobczak, S. (2024). Can Eye Movement Desensitization and Reprocessing Improve Cognition in Older Adults With PTSD? A First Exploration. Journal of Geriatric Psychiatry and Neurology, 37(3), 206–221. https://doi.org/10.1177/08919887231207639
Honda, H., Ashizawa, R., Kiriyama, K., Take, K., Hirase, T., Arizono, S., & Yoshimoto, Y. (2022). Chronic pain in the frail elderly mediates sleep disorders and influences falls. Archives of Gerontology and Geriatrics, 99, 104582. https://doi.org/10.1016/j.archger.2021.104582
Janssen, E. P., Spauwen, P. J., Rijnen, S. J., & Ponds, R. W. (2023). Exploration of EMDR in treating PTSD in patients with acquired brain injury: A retrospective case series. European Journal of Psychotraumatology, 14(2), 2264117. https://doi.org/10.1080/20008066.2023.2264117
Kalantar Qureshi, M., Barjalee, A., Zamayad, A., & Dartaj, F. (2012). The effectiveness of relaxation training and exercises on anxiety and working memory capacity. Quarterly Journal of Clinical Psychology Studies, 3(6), 65–88. https://jcps.atu.ac.ir/article_2061.html
Kamali-Nasab, Z., Koushki, S., Bani-Jamali, S. A., & Ourki, M. (2022). A comparison of the effectiveness of cognitive-behavioral therapy and mindfulness on sleep quality and cognitive abilities in women with insomnia. Clinical Psychology Studies, 12(48), 57–84. https://jcps.atu.ac.ir/article_15407.html
Li, J., Cao, Y., Ou, S., Jiang, T., Wang, L., & Ma, N. (2024). The effect of total sleep deprivation on working memory: evidence from diffusion model. Sleep, 47(2), zsae006. https://doi.org/10.1093/sleep/zsae006
Madani, S., Alizadeh, H., Farkhi, N., & Hakimi, A. (2017). Development of an executive functions training program and evaluation of its effectiveness in reducing symptoms in children with ADHD. Psychology of Exceptional Individuals, 7(26), 1–25. https://jpe.atu.ac.ir/article_7860.html
Mehrmanesh, A., Hafezi, F., Ehteshamzadeh, P., & Bakhtiarpour, S. (2023). A comparison of CBT, EMDR, and biofeedback on migraine attacks, anxiety sensitivity, and sleep and life quality. Health and Treatment Management, 14(3), 19–35. https://www.sid.ir/paper/1442715/fa
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex "frontal lobe" tasks: A latent variable analysis. Cognitive Psychology, 41(1), 49–100. https://doi.org/10.1006/cogp.1999.0734
Nelson, K. L., Davis, J. E., & Corbett, C. F. (2022). Sleep quality: An evolutionary concept analysis. Nursing Forum, 57(1), 144–151. https://doi.org/10.1111/nuf.12659
Nikro, B., Shahabi-Zadeh, F., & Nasri, M. (2022). The effectiveness of MBCT and ACT on sleep quality in students with test anxiety. Journal of Mental Health Principles, 24(6), 383–390. https://jfmh.mums.ac.ir/article_21464.html
Ong, J. C., Shapiro, S. L., & Manber, R. (2009). Mindfulness meditation and cognitive behavioral therapy for insomnia: a naturalistic 12-month follow-up. EXPLORE, 5(1), 30–36. https://doi.org/10.1016/j.explore.2008.10.004
Peng, Z., Hou, Y., Xu, L., Wang, H., Wu, S., Song, T., Shao, Y., & Yang, Y. (2023). Recovery sleep attenuates impairments in working memory following total sleep deprivation. Frontiers in Neuroscience, 17, 1056788. https://doi.org/10.3389/fnins.2023.1056788
Perrault, A. A., Pomares, F. B., Smith, D., Cross, N. E., Gong, K., Maltezos, A., McCarthy, M., Madigan, E., Tarelli, L., McGrath, J. J., & Savard, J. (2022). Effects of cognitive behavioral therapy for insomnia on subjective and objective measures of sleep and cognition. Sleep Medicine, 97, 13. https://doi.org/10.1016/j.sleep.2022.05.010
Peters, A. L., Saunders, W. J., & Jackson, M. L. (2022). Mindfulness-based strategies for improving sleep in people with psychiatric disorders. Current psychiatry reports, 24(11), 645–660. https://doi.org/10.1007/s11920-022-01370-z
Ranjbaripour, T., Hashemian, K., Ahadi, H., Rezabakhsh, H., & Farkhi, N. (2014). The effectiveness of eye movement desensitization and reprocessing (EMDR) therapy on primary insomnia. Clinical Psychology Studies, 4(15), 127–140. https://jcps.atu.ac.ir/article_348.html
Safaeyan, S., Pournaghash-Tehrani, S., Gholam-Ali Lavasani, M., & Abdoli-Bidehendi, M. (2023). The effectiveness of EMDR therapy on PTSD symptoms in patients undergoing coronary artery bypass graft surgery. Journal of Psychological Sciences, 22(127), 1303–1318. https://psychologicalscience.ir/article-1-1811-fa.html
Segal, Z. V., Teasdale, J. D., Williams, J. M., & Gemar, M. C. (2002). The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology & Psychotherapy, 9(2), 131–138. https://doi.org/10.1002/cpp.320
Shapiro, F. (1989). Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. Journal of Traumatic Stress, 2(2), 199–223. https://doi.org/10.1002/jts.2490020207
Shapiro, F. (2014). The role of EMDR therapy in medicine: addressing psychological and physical symptoms stemming from adverse life experiences. The Permanente Journal, 18(1), 71. https://doi.org/10.7812/TPP/13-098
Vahedi, S., Mirnasab, M., Fathi-Azar, E., & Damghani-MirMahalleh, M. (2019). The effect of mindfulness-based cognitive therapy on executive functioning and the reduction of oppositional defiant disorder symptoms in students. Sabzevar University of Medical Sciences Journal, 26(6), 709–718. https://sid.ir/paper/365817/fa
van den Hout, M. A., Engelhard, I. M., Beetsma, D., Slofstra, C., Hornsveld, H., Houtveen, J., & Leer, A. (2011). EMDR and mindfulness: Eye movements and attentional breathing tax working memory and reduce vividness and emotionality of aversive ideation. Journal of Behavior Therapy and Experimental Psychiatry, 42(4), 423–431. https://doi.org/10.1016/j.jbtep.2011.03.004
Virgilio, E., Solara, V., Sarnelli, M. F., Vecchio, D., & Comi, C. (2022). Early successful EMDR therapy for verbal memory impairment in an adjustment disorder: a case report in a newly-diagnosed multiple sclerosis patient. Reports, 5(2), 17. https://doi.org/10.3390/reports5020017
Wardle-Pinkston, S., Slavish, D. C., & Taylor, D. J. (2019). Insomnia and cognitive performance: A systematic review and meta-analysis. Sleep Medicine Reviews, 48, 101205. https://doi.org/10.1016/j.smrv.2019.07.008
Whitfield, T., Barnhofer, T., Acabchuk, R., Cohen, A., Lee, M., Schlosser, M., Arenaza-Urquijo, E. M., Böttcher, A., Britton, W., Coll-Padros, N., & Collette, F. (2022). The effect of mindfulness-based programs on cognitive function in adults: A systematic review and meta-analysis. Neuropsychology Review, 32(3), 677–702. https://doi.org/10.1007/s11065-021-09519-y
Zafar, U. e. H., Arshad, F., Karamat, A., Hayat, U., Khan, Z. K., & Ashraf, T. (2025). The Role of Working Memory in Problem-Solving and Decision-Making. Bbe, 14(2), 11-16. https://doi.org/10.61506/01.00586
Zhang, R., & Li, H. (2025). Effect of vigorous-intensity exercise on the working memory and inhibitory control among children with attention deficit hyperactivity disorder: a systematic review and meta-analysis. Italian Journal of Pediatrics, 51(1), 104. https://doi.org/10.1186/s13052-025-01924-w
Zioga, T., Ferentinos, A., Konsolaki, E., Nega, C., & Kourtesis, P. (2025). Video Game Skills Across Diverse Genres and Cognitive Functioning in Early Adulthood: Verbal and Visuospatial Short-Term and Working Memory, Hand–Eye Coordination, and Empathy. https://doi.org/10.31234/osf.io/e75cd