The Effect of Healthy Lifestyle Education Combined with Mindfulness-Based Stress Reduction on Health Anxiety and Health Dimensions in Pregnant Women at Risk of Preeclampsia
Keywords:
Healthy Lifestyle, Mindfulness-Based Stress Reduction, Health Anxiety, Health Dimensions, Pregnant Women, PreeclampsiaAbstract
Objective: This study aimed to investigate the effect of healthy lifestyle education combined with mindfulness-based stress reduction (MBSR) on health anxiety and multidimensional health outcomes in this high-risk population.
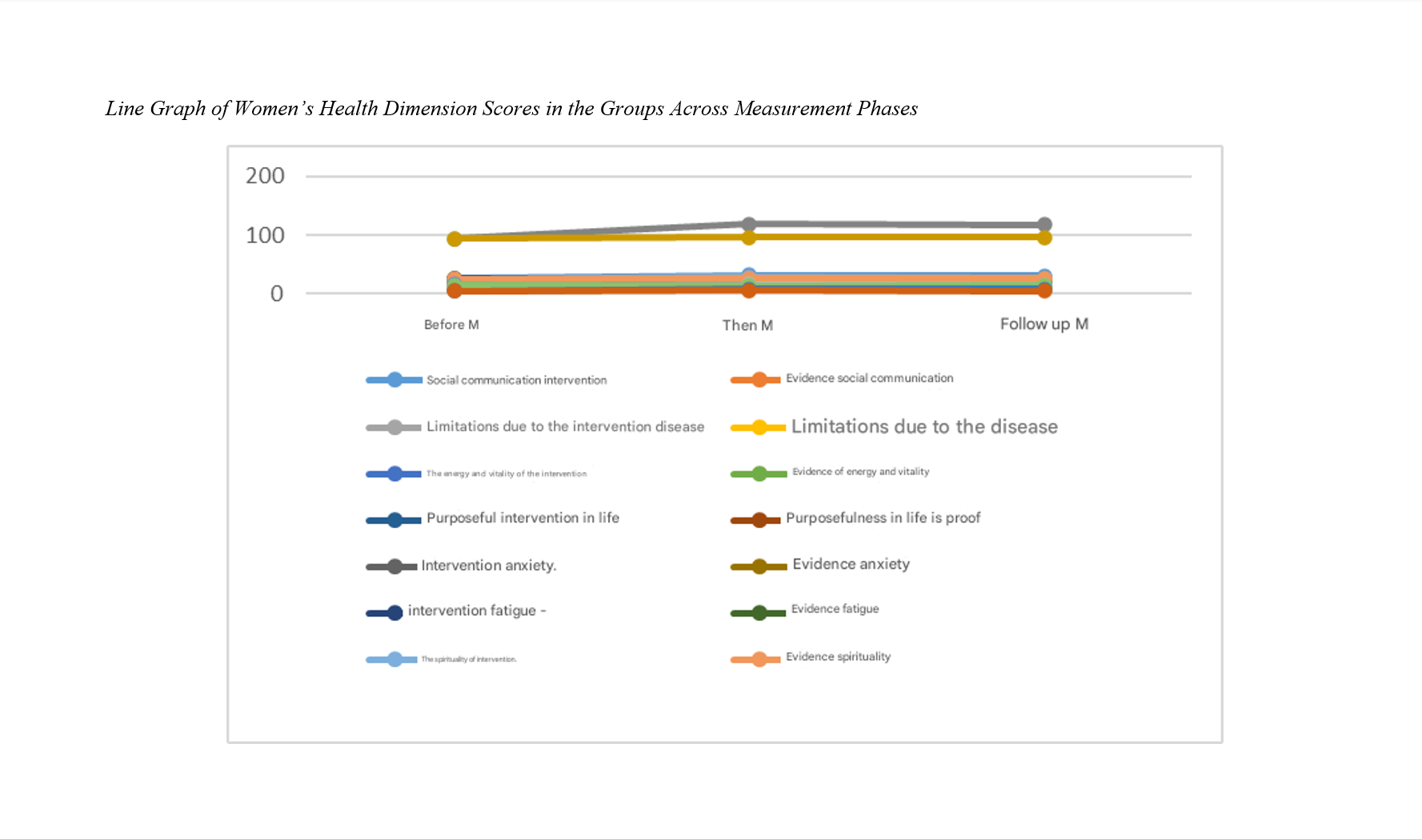
Methods and Materials: In this quasi-experimental study, 30 pregnant women at risk of preeclampsia were recruited from the Tolou Salamat Center in Tehran and randomly assigned to either an intervention group (n = 15) or a control group (n = 15). The intervention group participated in eight weekly sessions of lifestyle education integrated with mindfulness-based stress reduction, while the control group received no intervention. Participants completed validated questionnaires assessing health anxiety (HAI-18) and health dimensions (Four-Dimensional Health Scale) at baseline, post-intervention, and 1.5-month follow-up. Data were analyzed using repeated measures ANOVA and multivariate analysis of covariance.
Findings: The intervention led to a statistically significant reduction in health anxiety scores and sustained improvements across multiple health domains—including psychological, social, physical, and spiritual well-being—compared to the control group (p < 0.001). Key health anxiety indicators, such as perceived likelihood of illness and general health concerns, decreased substantially and these benefits persisted at follow-up. Similarly, significant gains were observed in total health scores and specific dimensions of quality of life, with the intervention explaining a considerable proportion of variance in outcomes.
Conclusion: Healthy lifestyle education combined with mindfulness-based stress reduction is an effective intervention for reducing health anxiety and enhancing multidimensional health among pregnant women at risk for preeclampsia. Integration of such programs into standard prenatal care—especially for high-risk populations—is recommended.
Downloads
References
Akbarzadeh, M., & Ahmadinezhad, F. (2019). Investigating the relationship of spiritual wellbeing with perceived stress and perceived social support among women with preeclampsia. Health, Spirituality and Medical Ethics, 6(4), 2-9. https://doi.org/10.29252/jhsme.6.4.2
Alexander, B., & Vladislav, B. (2015). Structure and content of the educational technology of managing students' healthy lifestyle. Journal of Physical Education and Sport, 15(3), 362. https://doi.org/10.7752/jpes.2015.03054
Armstrong, T. (2019). Backtalk: Keep religion out of mindfulness. Phi Delta Kappan, 101(4), 72. https://doi.org/10.1177/0031721719892986
Bahrami Ehsan, H., Saadati, M., & Mahmoudi, F. (2015). Structural structure of the four-dimensional health assessment questionnaire; biological-psychological-social-spiritual model. Journal of Behavioral Sciences Research, 13(2), 251-265. https://rbs.mui.ac.ir/article-1-401-fa.pdf
Bergeron, J., Avraam, D., Calas, L., Fraser, W., Harris, J. R., Heude, B., & Andersen, A. M. N. (2024). Stress and anxiety during pregnancy and length of gestation: a federated study using data from five Canadian and European birth cohorts. European Journal of Epidemiology, 39(7), 773-783. https://doi.org/10.1007/s10654-024-01126-4
Bernad, B. C., Tomescu, M. C., Velimirovici, D. E., Andor, M., Lungeanu, D., Enătescu, V., & Hogea, L. (2025). Impact of Stress and Anxiety on Cardiovascular Health in Pregnancy: A Scoping Review. Journal of clinical medicine, 14(3), 909. https://doi.org/10.3390/jcm14030909
Bisson, C., Dautel, S., Patel, E., Suresh, S., Dauer, P., & Rana, S. (2023). Preeclampsia pathophysiology and adverse outcomes during pregnancy and postpartum. Frontiers in Medicine, 10, 485. https://doi.org/10.3389/fmed.2023.1144170
Cong, X., Wang, J., Yang, L., Cui, L., Hua, Y., & Gong, P. (2025). Pregnancy stress in women at high risk of preeclampsia with their anxiety, depression, self-management capacity: a cross-sectional study. Frontiers in psychology, 16, 1537858. https://doi.org/10.3389/fpsyg.2025.1537858
Freire, V. A. F., de Melo, A. D., de Lima Santos, H., & de Barros Pinheiro, M. (2023). Evaluation of oxidative stress markers in subtypes of preeclampsia: A systematic review and meta-analysis. Placenta. https://doi.org/10.1016/j.placenta.2022.12.009
Gill, L. N., Renault, R., Campbell, E., Rainville, P., & Khoury, B. (2020). Mindfulness induction and cognition: A systematic review and meta-analysis. Consciousness and Cognition, 84, 102991. https://doi.org/10.1016/j.concog.2020.102991
Goetz, M., Schiele, C., Müller, M., Matthies, L. M., Deutsch, T. M., Spano, C., & Wallwiener, S. (2020). Effects of a brief electronic mindfulness-based intervention on relieving prenatal depression and anxiety in hospitalized high-risk pregnant women: exploratory pilot study. Journal of medical Internet research, 22(8), 17593. https://doi.org/10.2196/17593
Han, Y., Gao, X., Wang, X., Zhang, C., Gong, B., Peng, B., & Shan, Z. (2023). A systematic review and meta-analysis examining the risk of adverse pregnancy and neonatal outcomes in women with isolated hypothyroxinemia in pregnancy. Thyroid, 33(5), 603-614. https://doi.org/10.1089/thy.2022.0600
Jung, E., Romero, R., Yeo, L., Gomez-Lopez, N., Chaemsaithong, P., Jaovisidha, A., & Erez, O. (2022). The etiology of preeclampsia. American Journal of Obstetrics and Gynecology, 226(2), S844-S866. https://doi.org/10.1016/j.ajog.2021.11.1356
Lacks, M., Lamson, A., & Goodman, J. (2022). Biological, psychological, social, and spiritual health of active duty women: An exploratory study. Journal of Military, Veteran and Family Health, 8(1), 90-101. https://doi.org/10.3138/jmvfh-2021-0008
Lagerweij, G. R., Brouwers, L., De Wit, G. A., Moons, K. G. M., Benschop, L., Maas, A. H., & Koffijberg, H. (2020). Impact of preventive screening and lifestyle interventions in women with a history of preeclampsia: A micro-simulation study. European Journal of Preventive Cardiology, 27(13), 1389-1399. https://doi.org/10.1177/2047487319898021
Liu, C. H., Zhang, H. Y., Wang, F., Mu, S. S., & Wen, F. Y. (2025). Anxiety and hypertensive disorders of pregnancy: Epidemiology, mechanisms, and management strategies. World journal of psychiatry, 15(6), 105944. https://doi.org/10.5498/wjp.v15.i6.105944
Miller, E. C., Wilczek, A., Bello, N. A., Tom, S., Wapner, R., & Suh, Y. (2022). Pregnancy, preeclampsia and maternal aging: From epidemiology to functional genomics. Ageing Research Reviews, 73, 101535. https://doi.org/10.1016/j.arr.2021.101535
Moufarrej, M. N., Vorperian, S. K., Wong, R. J., Campos, A. A., Quaintance, C. C., Sit, R. V., & Quake, S. R. (2022). Early prediction of preeclampsia in pregnancy with cell-free RNA. Nature, 602(7898), 689-694. https://doi.org/10.1038/s41586-022-04410-z
Overdijkink, S. B., Velu, A. V., Rosman, A. N., Van Beukering, M. D., Kok, M., & Steegers-Theunissen, R. P. (2018). The usability and effectiveness of mobile health technology-based lifestyle and medical intervention apps supporting health care during pregnancy: systematic review. Jmir Mhealth and Uhealth, 6(4), e8834. https://doi.org/10.2196/mhealth.8834
Pishdadian, A., Shahreki, B., & Soltani, S. (2023). Mean corpuscular volume: a noninvasive marker in assessing pregnancy-induced hypertension and disease severity in preeclamptic patients. Iranian Journal of Obstetrics, Gynecology and Infertility.
Psilopatis, I., Vrettou, K., Fleckenstein, F. N., & Theocharis, S. (2023). The Role of Peroxisome Proliferator-Activated Receptors in Preeclampsia. Cells, 12(4), 647. https://doi.org/10.3390/cells12040647
Rahmani Fard, T., Kalantarkousheh, S. M., & Faramarzi, M. (2017). The effect of mindfulness-based cognitive psychotherapy on quality of life in infertile women. Hayat, 23(3), 277-289. https://hayat.tums.ac.ir/article-1-2024-fa.html
Reusch, A., Ströbl, V., Ellgring, H., & Faller, H. (2011). Effectiveness of small-group interactive education vs. lecture-based information-only programs on motivation to change and lifestyle behaviours. A prospective controlled trial of rehabilitation inpatients. Patient Education and Counseling, 82(2), 186-192. https://doi.org/10.1016/j.pec.2010.04.031
Roberts, L., Henry, A., Harvey, S. B., Homer, C. S., & Davis, G. K. (2022). Depression, anxiety and posttraumatic stress disorder six months following preeclampsia and normotensive pregnancy: a P4 study. BMC Pregnancy and Childbirth, 22(1), 108. https://doi.org/10.1186/s12884-022-04439-y
Salkovskis, P. M., Rimes, K. A., Warwick, H. M. C., & Clark, D. (2002). The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological medicine, 32(5), 843-853. https://doi.org/10.1017/S0033291702005822
San Juan-Reyes, S., Gómez-Oliván, L. M., San Juan-Reyes, N., Islas-Flores, H., Dublán-García, O., Orozco-Hernández, J. M., & Mejía-García, A. (2023). Women with preeclampsia exposed to air pollution during pregnancy: Relationship between oxidative stress and neonatal disease-Pilot study. Science of The Total Environment, 871, 161858. https://doi.org/10.1016/j.scitotenv.2023.161858
Sanaati, F., Mohammad-Alizadeh, S., Mirghafourvand, M., Alizadeh Sharjabadi, F., & Galeshi, M. (2018). The Effect of training pregnant women and their husbands on health promoting behaviors during pregnancy and postpartum period. Journal of Babol University of Medical Sciences, 20(5), 38-47. https://jbums.org/article-1-7029-fa.html
Santorelli, S. F., Kabat-Zinn, J., Blacker, M., Meleo-Meyer, F., & Koerbel, L. (2017). Mindfulness-Based Stress Reduction (MBSR): Authorized Curriculum Guide. Center for Mindfulness in Medicine, Health Care, and Society, University of Massachusetts Medical School. https://www.tarkustekool.ee/wp-content/uploads/2021/09/CFM-Teaching-UMass-MBSR-Curriculum-Teaching-Guide-2017.pdf
Schuman-Olivier, Z., Trombka, M., Lovas, D. A., Brewer, J. A., Vago, D. R., Gawande, R., Dunne, J. P., Lazar, S. W., Loucks, E. B., & Fulwiler, C. (2020). Mindfulness and Behavior Change. Harvard Review of Psychiatry, 28(6), 371-394. https://doi.org/10.1097/HRP.0000000000000277
Shahoie, R., Karimi, A., Sharifish, S., Soufizadeh, N., & Khanpour, F. (2019). Evaluation of the effectiveness of mindfulness-based stress reduction on anxiety in pregnant women. Scientific Journal of Nursing, Midwifery and Paramedical Faculty, 5(3), 83-94. https://sjnmp.muk.ac.ir/article-1-271-fa.html
Sinha, T., Brushett, S., Prins, J., & Zhernakova, A. (2023). The maternal gut microbiome during pregnancy and its role in maternal and infant health. Current Opinion in Microbiology, 74, 102309. https://doi.org/10.1016/j.mib.2023.102309
Song, Y., & Lindquist, R. (2015). Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Education Today, 35(1), 86-90. https://doi.org/10.1016/j.nedt.2014.06.010
Tian, Y., Zhou, Q., Zhang, L., Li, W., Yin, S., Li, F., & Xu, C. (2023). In utero exposure to per-/polyfluoroalkyl substances (PFASs): Preeclampsia in pregnancy and low birth weight for neonates. Chemosphere, 313, 137490. https://doi.org/10.1016/j.chemosphere.2022.137490
Wang, H., Zhang, Z., Li, H., Li, J., Li, H., Liu, M., & Zuo, Y. (2023). A cost-effective machine learning-based method for preeclampsia risk assessment and driver genes discovery. Cell & Bioscience, 13(1), 41. https://doi.org/10.1186/s13578-023-00991-y