Analysis of Interpretation Bias Related to Overeating in Obese Individuals with Weight Loss Surgery: A Qualitative Study
Keywords:
Interpretation Bias, Obesity, Weight LossAbstract
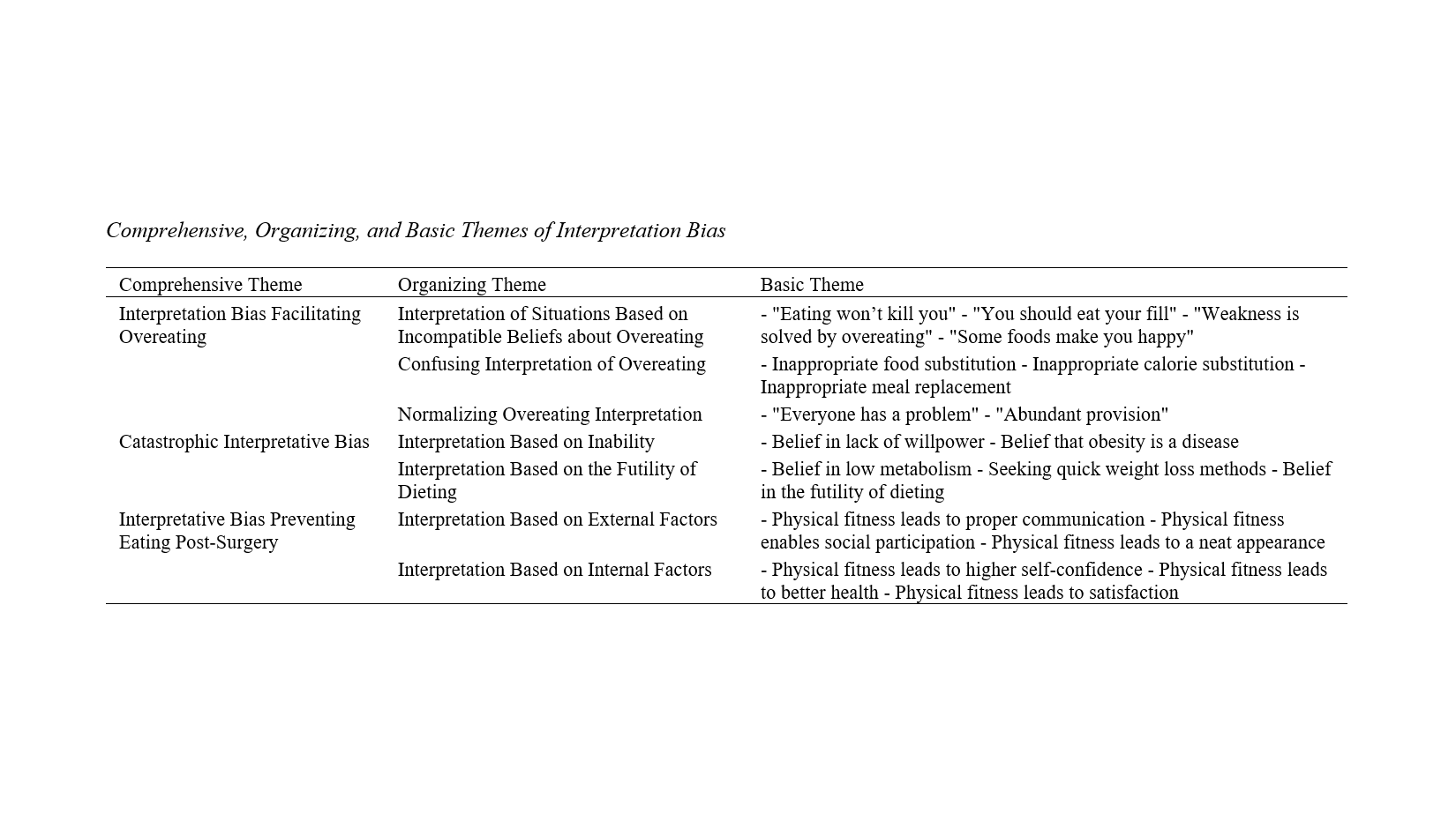
This study aimed to analyze interpretation bias related to overeating in obese individuals following weight loss surgery. The research type was qualitative and utilized the thematic analysis method of Clarke and Braun (2006). The research environment included all individuals with a history of obesity and weight loss surgery. Participants were ten individuals selected purposefully. The criterion for the number of participants was data saturation. The research tool was a semi-structured interview with questions related to interpretation bias in this group. Data were analyzed using Clarke and Braun’s (2006) six-step method. The results showed that interpretation bias among these individuals consisted of three overarching categories: 1) Interpretative bias facilitating overeating (with organizing codes of interpreting situations based on incompatible beliefs about overeating, normalizing overeating, and confusing interpretations of overeating), 2) Catastrophic interpretative bias (with organizing categories of interpretative bias based on inability and interpretative bias based on the futility of dieting), and 3) Interpretative bias inhibiting eating (with organizing categories of interpretative bias based on external issues and interpretative bias based on internal issues). Based on the results of this study, it can be said that to prevent overeating or maintain weight loss, individuals prone to or suffering from overeating need to manage their cognitive biases and receive training in this area.
Downloads
References
1. Saad F, Doros G, Haider KS, Haider A. Differential effects of 11 years of long-term injectable testosterone undecanoate therapy on anthropometric and metabolic parameters in hypogonadal men with normal weight, overweight and obesity in comparison with untreated controls: real-world data from a controlled registry study. International Journal of Obesity. 2020;44(6):1264-78. [PMID: 32060355] [PMCID: PMC7260126] [DOI]
2. Li G, Hu Y, Zhang W, Wang J, Ji W, Manza P, et al. Brain functional and structural magnetic resonance imaging of obesity and weight loss interventions. Molecular Psychiatry. 2023;28(4):1466-79. [PMID: 36918706] [PMCID: PMC10208984] [DOI]
3. Smeets E, Roefs A, van Furth E, Jansen A. Attentional bias for body and food in eating disorders: Increased distraction, speeded detection, or both? Behaviour Research and Therapy. 2008;46(2):229-38. [PMID: 18191812] [DOI]
4. Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The Effectiveness of Telemental Health: A 2013 Review. Telemedicine and e-Health. 2013;19(6):444-54. [PMID: 23697504] [PMCID: PMC3662387] [DOI]
5. Ivezaj V, Grilo CM. The complexity of body image following bariatric surgery: a systematic review of the literature. Obesity Reviews. 2018;19(8):1116-40. [PMID: 29900655] [PMCID: PMC6296375] [DOI]
6. Gentileschi P, Bianciardi E, Siragusa L, Tognoni V, Benavoli D, D’Ugo S. Banded Sleeve Gastrectomy Improves Weight Loss Compared to Nonbanded Sleeve: Midterm Results from a Prospective Randomized Study. Journal of Obesity. 2020;2020(1):9792518. [PMID: 32566276] [PMCID: PMC7285409] [DOI]
7. Schroeder R, HARRISON DT, McGRAW SL. Treatment of adult obesity with bariatric surgery. American family physician. 2016;93(1):31-7.
8. Sherf-Dagan S, Sinai T, Goldenshluger A, Globus I, Kessler Y, Schweiger C, et al. Nutritional Assessment and Preparation for Adult Bariatric Surgery Candidates: Clinical Practice. Advances in Nutrition. 2021;12(3):1020-31. [PMID: 33040143] [PMCID: PMC8262552] [DOI]
9. Mechanick JI, Apovian C, Brethauer S, Timothy Garvey W, Joffe AM, Kim J, et al. Clinical Practice Guidelines for the Perioperative Nutrition, Metabolic, and Nonsurgical Support of Patients Undergoing Bariatric Procedures – 2019 Update: Cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic and Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Obesity. 2020;28(4):O1-O58. [DOI]
10. Sudlow A, le Roux CW, Pournaras DJ. The metabolic benefits of different bariatric operations: what procedure to choose? Endocrine Connections. 2020;9(2):R28-R35. [PMID: 31917678] [PMCID: PMC6993254] [DOI]
11. Mahmoodianfard S, Haghighat N. The Psychosocial Determinants of Obesity Associated with Food Intake (Narrative Review). Journal of Health Sciences & Surveillance System. 2023;11(1):2-8.
12. Lowe CJ, Reichelt AC, Hall PA. The Prefrontal Cortex and Obesity: A Health Neuroscience Perspective. Trends in Cognitive Sciences. 2019;23(4):349-61. [PMID: 30824229] [DOI]
13. Brooks S, Prince A, Stahl D, Campbell IC, Treasure J. A systematic review and meta-analysis of cognitive bias to food stimuli in people with disordered eating behaviour. Clinical Psychology Review. 2011;31(1):37-51. [PMID: 21130935] [DOI]
14. Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle Modification for Obesity. Circulation. 2012;125(9):1157-70. [PMID: 22392863] [PMCID: PMC3313649] [DOI]
15. Zhou A, Xie P, Ahmed MZ, Jobe MC, Ahmed O. Body mass index and attention bias of food cues in women: a mediation model of body weight dissatisfaction. PeerJ. 2022;10:e13863. [DOI]
16. Vreeken D, Seidel F, Custers EM, Olsthoorn L, Cools S, Aarts EO, et al. Factors Associated With Cognitive Improvement After Bariatric Surgery Among Patients With Severe Obesity in the Netherlands. JAMA Network Open. 2023;6(5):e2315936-e. [PMID: 37252738] [PMCID: PMC10230316] [DOI]
17. Dardano A, Aghakhanyan G, Moretto C, Ciccarone A, Bellini R, Sancho Bornez V, et al. Brain effect of bariatric surgery in people with obesity. International Journal of Obesity. 2022;46(9):1671-7. [PMID: 35729365] [DOI]
18. Eklund AA, Helmefalk M. Congruency or incongruency: a theoretical framework and opportunities for future research avenues. Journal of Product & Brand Management. 2022;31(4):606-21. [DOI]
19. Stice E, Rohde P, Gau JM, Butryn ML, Shaw H, Cloud K, et al. Enhancing efficacy of a dissonance-based obesity and eating disorder prevention program: Experimental therapeutics. Journal of Consulting and Clinical Psychology. 2021;89(10):793-804. [PMID: 34807655] [PMCID: PMC9447345] [DOI]
20. Yahya AH, Sukmayadi V. A review of cognitive dissonance theory and its relevance to current social issues. MIMBAR: Jurnal Sosial Dan Pembangunan. 2020;36(2):480-8. [DOI]
21. Kornacka M, Czepczor-Bernat K, Napieralski P, Brytek-Matera A. Rumination, mood, and maladaptive eating behaviors in overweight and healthy populations. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 2021;26(1):273-85. [PMID: 32072571] [PMCID: PMC7895787] [DOI]
Downloads
Additional Files
Published
License
Copyright (c) 2024 Samira Tavakoli Kohpaei (Author); Hajar Torkan (Corresponding Author); Zahra Yousefi (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.