The Effect of Aerobic and Resistance Training on Gut Microbiome Composition and Its Association with Irisin Protein Levels in Aged Mice: The Role of Faecalibacterium prausnitzii, Clostridium difficile, and Enterococcus faecalis
Keywords:
Gut microbiome, Irisin, Resistance training, Aerobic training, AgingAbstract
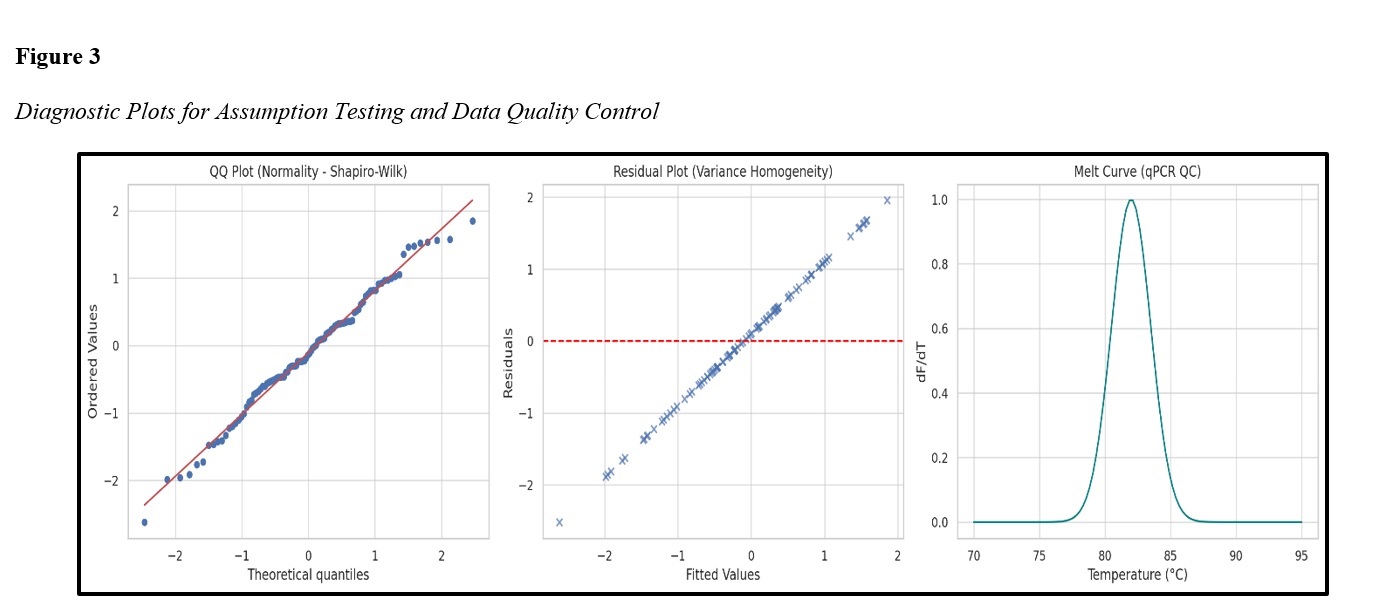
In the aging period, alterations in gut microbiome composition and the decline of myokine proteins—such as irisin—are considered major contributors to metabolic disorders, inflammatory conditions, and muscle weakness. In this context, the role of exercise interventions in simultaneously modulating these two biological indicators has gained increasing attention. The present study aimed to examine the effects of aerobic and resistance training on gut microbiome composition and plasma irisin levels in aged mice, with a focus on three key species: Faecalibacterium prausnitzii, Clostridium difficile, and Enterococcus faecalis. This experimental study was conducted over eight weeks on 40 male Wistar rats assigned to five groups: young control, aged without training, sham, aerobic training, and resistance training. Plasma irisin levels were measured using the ELISA method, and the relative abundance of bacteria was assessed using real-time polymerase chain reaction (qPCR). Data were analyzed using multifactorial ANOVA and Tukey’s post hoc test. The results indicated that aerobic and resistance training led to a significant increase in plasma irisin levels in aged mice compared with the inactive group. Resistance training showed the greatest increase. Additionally, the abundance of F. prausnitzii increased in the trained groups, while the abundance of C. difficile and E. faecalis decreased. Composite microbial health indices (F/BAD, F/Cd, F/Ef) also improved significantly. A positive association between irisin levels and microbial ratios was confirmed. The findings suggest that physical exercise—particularly resistance training—can simultaneously enhance gut microbiome composition and myokine status in the elderly. These results support the central role of the “gut–muscle axis” in the physiological response to exercise and provide a basis for designing personalized training interventions in geriatric medicine.
Downloads
References
1. Marchesi JR, Adams DH, Fava F, Hermes GDA, Hirschfield GM, Hold G, et al. The gut microbiota and host health: A new clinical frontier. Gut. 2016;65(2):330-9. [PMID: 26338727] [PMCID: PMC4752653] [DOI]
2. Picca A, Fanelli F, Calvani R, Mulè G, Pesce V, Sisto A, et al. Gut dysbiosis and muscle aging: Searching for novel targets against sarcopenia. Mediators of Inflammation. 2018;2018:7026198. [PMID: 29686533] [PMCID: PMC5893006] [DOI]
3. Kirschner C, Rink L. Gut microbiota composition and sarcopenia: Decreased SCFA-producing bacteria in elderly subjects. Frontiers in Microbiology. 2025;16:1532.
4. Ticinesi A, Lauretani F, Tana C, Nouvenne A, Ridolo E, Meschi T. Exercise and immune system as modulators of intestinal microbiome: Implications for the gut-muscle axis hypothesis. Exercise Immunology Review. 2019;25:84-95.
5. Langsetmo L, Johnson A, Demmer RT, Fino N, Orwoll ES, Ensrud KE, et al. The association between objectively measured physical activity and the gut microbiome among older community-dwelling men. The Journal of Nutrition, Health & Aging. 2019;23(6):538-46. [PMID: 31233075] [PMCID: PMC6618308] [DOI]
6. Frontiers in M. Age-related dysbiosis and loss of SCFA-producing bacteria: Implications for metabolic health. Frontiers in Microbiology. 2025;16:1882.
7. Allam-Ndoul B, Castonguay-Paradis S, Veilleux A. Gut microbiota and intestinal trans-epithelial permeability. International Journal of Molecular Sciences. 2020;21(17):6402. [PMID: 32899147] [PMCID: PMC7503654] [DOI]
8. Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux JJ, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proceedings of the National Academy of Sciences. 2008;105(43):16731-6. [PMID: 18936492] [PMCID: PMC2575488] [DOI]
9. Martín R, Miquel S, Ulmer J, Kechaou N, Langella P, Bermúdez-Humarán LG. The role of Faecalibacterium prausnitzii in health and disease. GeroScience. 2023;45(3):827-44.
10. Taniguchi H, Soga T, Satoh M. Endurance exercise training reduces Clostridium difficile abundance and improves gut health in elderly men. Journal of Applied Physiology. 2018;125(4):1066-74.
11. Lengfelder I, Sava IG, Hansen J. Enterococcus faecalis and inflammatory bowel disease: Pathophysiology and therapeutic targets. Gut Microbes. 2019;10(3):370-82.
12. Przewłócka K, Folwarski M, Kaźmierczak-Siedlecka K, Skonieczna-Żydecka K, Kaczor JJ. Gut-muscle axis exists and may affect skeletal muscle adaptation to training. Nutrients. 2020;12(5):1451. [PMID: 32443396] [PMCID: PMC7285193] [DOI]
13. Mitchell CM, Davy BM, Hulver MW, Neilson AP, Bennett BJ, Davy KP. Does exercise alter gut microbial composition? A systematic review. Medicine & Science in Sports & Exercise. 2019;51(1):160-7. [PMID: 30157109] [DOI]
14. Allen JM, Mailing LJ, Niemiro GM, Moore R, Cook MD, White BA, et al. Exercise alters gut microbiota composition and function in lean and obese humans. Medicine & Science in Sports & Exercise. 2018;50(4):747-57. [PMID: 29166320] [DOI]
15. Mach N, Fuster-Botella D. Endurance exercise and gut microbiota: A review. Journal of Sport and Health Science. 2017;6(2):179-97. [PMID: 30356594] [PMCID: PMC6188999] [DOI]
16. Aya V, Flórez A, Perez L, Ramírez JD. Association between physical activity and changes in intestinal microbiota composition: A systematic review. PLoS ONE. 2021;16(2):e0247039. [PMID: 33630874] [PMCID: PMC7906424] [DOI]
17. Ortiz-Alvarez L, Xu H, Martinez-Tellez B. Influence of exercise on the human gut microbiota of healthy adults: A systematic review. Clinical and Translational Gastroenterology. 2020;11(2):e00126. [PMID: 32463624] [PMCID: PMC7145029] [DOI]
18. Dorelli B, Gallè F, De Vito C, Duranti G, Iachini M, Zaccarin M, et al. Can physical activity influence human gut microbiota composition independently of diet? A systematic review. Nutrients. 2021;13(6):1890. [PMID: 34072834] [PMCID: PMC8228232] [DOI]
19. Clauss M, Gérard P, Mosca A, Leclerc M. Exercise and the gut microbiota: Implications for health and performance. Frontiers in Nutrition. 2021;8:637010. [PMID: 34179053] [PMCID: PMC8222532] [DOI]
20. Zhu Q, Jiang S, Du G. Effects of exercise frequency on the gut microbiota in elderly individuals. MicrobiologyOpen. 2020;9(8):e1053. [PMID: 32356611] [PMCID: PMC7424259] [DOI]
21. Ramos J, Silva A, Sousa N. Exercise-induced modulation of the gut microbiome in older adults: A systematic review. Aging and Disease. 2022;13(6):1789-803.
22. Castro-Mejía JL, Khakimov B, Krych Ł, Bülow J, Bechshøft RL, Højfeldt G, et al. Physical fitness in community-dwelling older adults is linked to dietary intake, gut microbiota, and metabolomic signatures. Aging Cell. 2020;19(3):e13105. [PMID: 31967716] [PMCID: PMC7059135] [DOI]
23. Giudici K, Bernard T, Chassaing B. Physical activity adherence associates with higher Faecalibacterium prausnitzii abundance in older adults: A geroscience approach. GeroScience. 2025;47(1):115-32.
24. Ma Y, Zhang J, Xu X. Aging reduces FNDC5/irisin expression in skeletal muscle: Implications for sarcopenia and exercise interventions. Experimental Gerontology. 2025;188:112516.
25. Liu W, Wang D, Yang X. FNDC5/irisin deficiency induces gut dysbiosis and depressive-like behavior in mice via the gut-brain axis. Molecular Psychiatry. 2023;28(3):1234-48.
26. Wang L, Xie Y, Zhang H. Irisin ameliorates osteoporosis and gut dysbiosis by enhancing intestinal barrier and modulating microbiota in ovariectomized mice. Bone Reports. 2025;24:101521.
27. Varghese RT, Hegde P, Ramasamy S. Impact of aerobic and resistance exercise on gut microbial diversity and SCFA production in healthy adults: A systematic review. Nutrients. 2024;16(5):985.
28. Goodarzi F, Nikbakht H, Abed Natanzi H, Ebrahim K, Ghazalian F. Comparison of the effects of aerobic and resistance training on oxidative indices and TGF-β in the cardiac tissue of aged mice. Razi Journal of Medical Sciences. 2020;27(3):93-102.
29. Esmaeili Seyrchi M, Banaei Boroujeni J, Mojtahhedi H, Saramī L. Distinct effects of aerobic versus resistance training on irisin levels and expression of inflammatory genes TGF-β, NF-κB, and SIRT1 in intestinal lymphocytes of aged mice. Longevity. 2025;3(2):1-18.
30. Kalantari A, Keshavarz S, Arab Momeni AY, Saramī L. Effects of high- and moderate-intensity aerobic interventions on gut microbiome diversity and function: examining changes in Lactobacillus, Bifidobacterium, and Escherichia coli in aged mice. Longevity. 2025;3(2):1-15.
31. Iwamoto J, Takeda TIS. Effect of exercise training and detraining on bone mineral density in postmenopausal women with osteoporosis. Journal of Orthopaedic Science. 2001;6(2):128-32. [PMID: 11484097] [DOI]
32. Horn MATA. Aging and the cardiac collagen matrix: Novel mediators of fibrotic remodeling. Journal of Molecular and Cellular Cardiology. 2016;175:175-85. [PMID: 26578393] [PMCID: PMC4945757] [DOI]