Ranking Cognitive–Affective Factors in the Development of Psychosomatic Illness
Keywords:
psychosomatic illness, emotional dysregulation, cognitive appraisal, stress reactivityAbstract
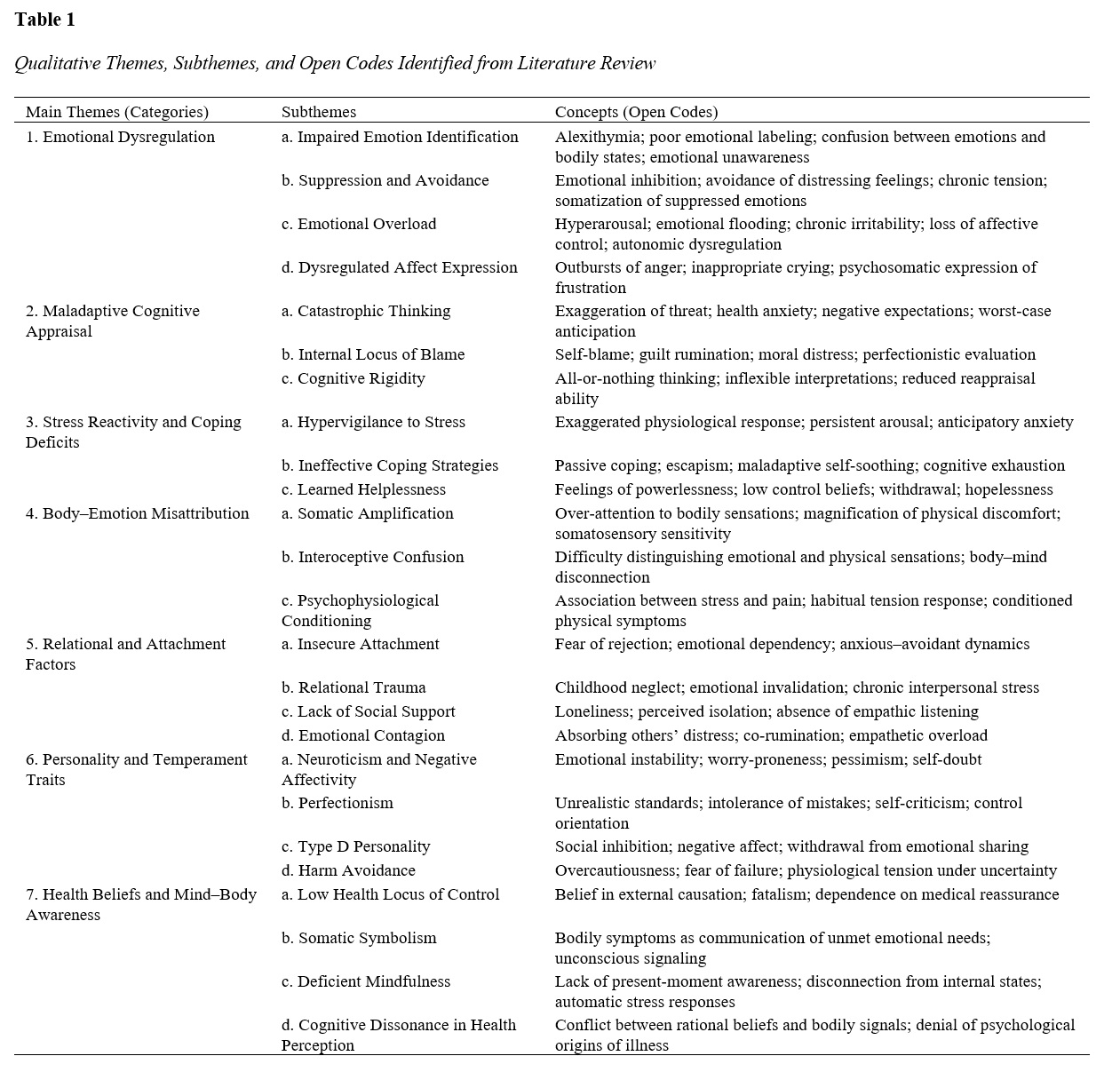
This study aimed to identify and rank the key cognitive–affective factors contributing to the development of psychosomatic illness through an integrated qualitative–quantitative research design. A mixed-methods sequential design was employed. In the qualitative phase, an extensive literature review of 127 scientific sources published between 2000 and 2025 was conducted to identify the principal cognitive–affective mechanisms underlying psychosomatic illness. Using NVivo 14 software, open and axial coding were applied until theoretical saturation was achieved, resulting in seven major thematic categories. In the quantitative phase, a structured questionnaire was developed based on these qualitative findings and administered to 288 adult participants from Portugal. Participants rated the importance of each factor on a 5-point Likert scale. The collected data were analyzed using SPSS version 26, with descriptive and inferential analyses determining the ranking and significance of each factor. The results showed that emotional dysregulation was the most influential factor contributing to psychosomatic illness (M = 4.62, SD = 0.43), followed by stress reactivity and coping deficits (M = 4.48, SD = 0.52) and maladaptive cognitive appraisal (M = 4.36, SD = 0.58). Relational and attachment factors ranked fourth (M = 4.27, SD = 0.61), while body–emotion misattribution and personality traits followed with moderate influence. Health beliefs and mind–body awareness received the lowest mean score (M = 3.89, SD = 0.67). Inferential analyses indicated statistically significant differences across demographic groups, with higher psychosomatic sensitivity observed among participants with greater emotional suppression and lower coping efficacy. The findings highlight emotional dysregulation and maladaptive stress processing as the most critical cognitive–affective determinants of psychosomatic illness. Interventions targeting emotion regulation, adaptive coping, and cognitive restructuring are essential to prevent and manage psychosomatic symptoms.
Downloads
References
Alsaffar, K. F. (2023). Overexcitability and Its Impact on Psychosomatic Disorders and the Role of "Cognitive Emotion Regulation" as a Mediating Variable. https://doi.org/10.21203/rs.3.rs-2397392/v1
Badaye, A., Vaziri, S., & Kashani, F. L. (2021). Developing a Psychosomatic Symptoms Model Based on Emotional Regulation, Defense Mechanisms, and Attachment Styles Mediated by Distress Level in Psychosomatic Patients. Hormozgan Medical Journal, 25(3), 98-103. https://doi.org/10.34172/hmj.2021.11
Basińska, M. A., & Woźniewicz, A. (2021). Diagnostic Criteria for Psychosomatic Research – Revised Version by Giovanni A. Fava and His Research Team. Psychiatria I Psychologia Kliniczna, 21(2), 121-127. https://doi.org/10.15557/pipk.2021.0013
Burlakova, I., & Шевяков, О. (2021). Socio-Psychological Technologies of Professional Health Formation. Public Administration and Law Review(3), 54-64. https://doi.org/10.36690/2674-5216-2021-3-54
Cheraghian, H., Kiani, A. R., Sharif, A. R., Ghivi, H. G., & Momeni, A. (2021). Emotion Regulation in Psychosomatic Diseases: Qualitative Study. Shenakht Journal of Psychology and Psychiatry, 8(1), 121-133. https://doi.org/10.32598/shenakht.8.1.121
Chystovska, Y., Bratanich, O., Zhurakovskyi, I., Akopian, A., & Ізвекова, О. Ю. (2022). Neuropsychological Correction of Psychosomatic Disorders. Brain Broad Research in Artificial Intelligence and Neuroscience, 13(1), 145-157. https://doi.org/10.18662/brain/13.1/273
Efremov, A. (2023). Eliminating Psychosomatic Pain and Negative Emotions With Dehypnosis. Journal of Organizational Behavior Research, 8(1), 1-11. https://doi.org/10.51847/rnrhuqmtqy
Farahi, S., Naziri, G., Davodi, A., & Fath, N. (2023). The Mediating Role of Cognitive Emotion Regulation Strategies in the Relationship Between Early Maladaptive Schemas, Alexithymia, and Emotional Intelligence With Somatic Symptoms in People With Somatic Symptoms Disorder. Practice in Clinical Psychology, 11(3), 187-200. https://doi.org/10.32598/jpcp.11.3.887.1
Fedorchuk, M. (2024). The Interaction Between Psychological Factors and Thyroid Disorders: A Psychosomatic Aspect. Kyiv Journal of Modern Psychology and Psychotherapy, 8, 147-161. https://doi.org/10.48020/mppj.2024.02.11
Feinstein, D. (2021). Applications of Energy Psychology in Addressing the Psychological Roots of Illness. Obm Integrative and Complementary Medicine, 06(02), 1-1. https://doi.org/10.21926/obm.icm.2102014
Gasparre, D., Pepe, I., Laera, D., Abbatantuono, C., De, M. F., Taurino, A., D’Erasmo, D., Fanizzi, P., Antonucci, L. A., Pantaleo, A., Cavallaro, G., Pontillo, V., Taurisano, P., & Quaranta, N. (2023). Cognitive Functioning and Psychosomatic Syndromes in a Subjective Tinnitus Sample. Frontiers in psychology, 14. https://doi.org/10.3389/fpsyg.2023.1256291
Hampannawar, P. R., & Patil, A. S. (2025). Role of Homoeopathy in Treating Psychosomatic Ailments and Restoration of Mental Health: Case Series. CDF, 54(3), 2742-2750. https://doi.org/10.48047/9w32nj35
Khan, A. H. (2022). The Impact of Sequencing Human Genome on the Psychosomatic Illnesses. J Can Res Rev Rep, 1-15. https://doi.org/10.47363/jcrr/2022(4)165
Kirat. (2025). The Gut-Brain Axis in Psychosomatic Disorders: A Biological Exploration of Mind-Body Interactions. Innovative Research Thoughts, 11(3), 54-60. https://doi.org/10.36676/irt.v11.i3.1647
Larionow, P., Агеенкова, Е. К., & Dedenok, M. I. (2022). Towards Psychosomatic Medicine: The Role of Age and Emotional Characteristics in People With Psychosomatic Disorders. Annales Universitatis Mariae Curie-Skłodowska Sectio J – Paedagogia-Psychologia, 35(3), 143-156. https://doi.org/10.17951/j.2022.35.3.143-156
Narmetova, Y., Kuldosheva, G., & Bekmirov, T. (2021). The Psychological Services Role in the Psychodiagnostics and Psychocorrection of Psychosomatic Patients in the Psychoemotional Situation. International Journal of Multicultural and Multireligious Understanding, 8(12), 249. https://doi.org/10.18415/ijmmu.v8i12.3277
Peixoto, A., Viana, G. R., Almeida, K. A. d., Karina Brito da Costa, O., Barbosa, P. G. P., Ivo, R. S., & Caldeira, A. G. (2024). O Impacto Das Doenças Psicossomáticas Na Saúde Mental Da Sociedade Pós Pandemia De Covid – 19. Lev, 15(41), 6075-6096. https://doi.org/10.56238/levv15n41-083
Pylypenko, N., Kovalova, O., Prokofieva, O., Kochkurova, O., Kriukova, M., & Zelinska, Y. (2022). Contemporary Approaches to Diagnosis, Psychotherapy and Neuro-Psychocorrection of Emotional Disorders in Psychosomatic Diseases. Brain Broad Research in Artificial Intelligence and Neuroscience, 13(1Sup1), 277-294. https://doi.org/10.18662/brain/13.1sup1/319
Pylypenko, N., Liasch, O., Chorna, I., Kompanovych, M., Levina, N., & Chystovska, Y. (2022). Neuropsychological Correction Technologies of Psychosomatic Disorders and Diseases. Brain Broad Research in Artificial Intelligence and Neuroscience, 13(2), 113-129. https://doi.org/10.18662/brain/13.2/335
Shahverdi, A., Omidi, M., & Nik, M. M. (2023). Effect of Mindfulness-Based Cognitive Therapy on Cognitive Emotion Regulation, Psychosomatic Symptom Severity of Migraine, and Stress Coping Styles of Women With Migraine. Iranian Journal of Psychiatry and Clinical Psychology, 29(1), 18-31. https://doi.org/10.32598/ijpcp.29.1.4414.1
Shoenberg, P. (2020). Developing a Psychosomatic Imagination in Medical Students and Psychotherapy Trainees. British Journal of Psychotherapy, 36(4), 597-609. https://doi.org/10.1111/bjp.12563
Sobennikov, V., Vinokurov, E. V., Рычкова, Л. В., & Sobennikova, V. V. (2019). Emotional Dysregulation as a Factor of Psychosomatic Disturbances in Depression and Cardiovascular Pathology (Analytical Review of Foreign Literature). Acta Biomedica Scientifica, 4(1), 87-92. https://doi.org/10.29413/abs.2019-4.1.13
Wagdy, E. (2024). Peercite Journal of Mental Health. Peercite J Ment Health, 2(S1), 576-594. https://doi.org/10.61641/pjmh.2024.2.s1.576-594
Yadlovska, O., Formaniuk, Y., Chystovska, Y., Nikolaiev, L. O., Boiaryn, L., & Матейко, Н. (2022). Neuropsychological Preventive Treatment of Emotional Burnout Among University Students. Brain Broad Research in Artificial Intelligence and Neuroscience, 13(1), 188-201. https://doi.org/10.18662/brain/13.1/276
Yoshiuchi, K. (2023). Psychosomatic Correlation in Hematopoietic Stem Cell Transplantation. Japanese Journal of Transplantation and Cellular Therapy, 12(3), 157-160. https://doi.org/10.7889/tct-23-006
Zhou, Y., & Yani, Z. (2024). Non-Adaptive Cognitive Emotion Regulation Mediates the Relationship Between Disease Uncertainty and Acute Stress Disorder in Patients With Ischaemic Stroke. Frontiers in Psychiatry, 15. https://doi.org/10.3389/fpsyt.2024.1319848
Кондратенко, А. П. (2020). Cognitive and Emotional Disturbances of Patients With Type II Diabetes Mellitus. Експериментальна І Клінічна Медицина, 89(4), 49-52. https://doi.org/10.35339/ekm.2020.89.04.07
Піонтковський, В., Візнюк, І., & Долинний, С. (2024). Psychosomatic Medicine: Health as a Key Element of Permanent Sustainable Life Affirmation. Сні(1(1)). https://doi.org/10.52058/3041-1572-2024-1(1)-13-21