Documenting the Physical and Psychological Consequences of COVID-19
Keywords:
Physical Consequences, Psychological Consequences, COVID-19, Grounded Theory MethodAbstract
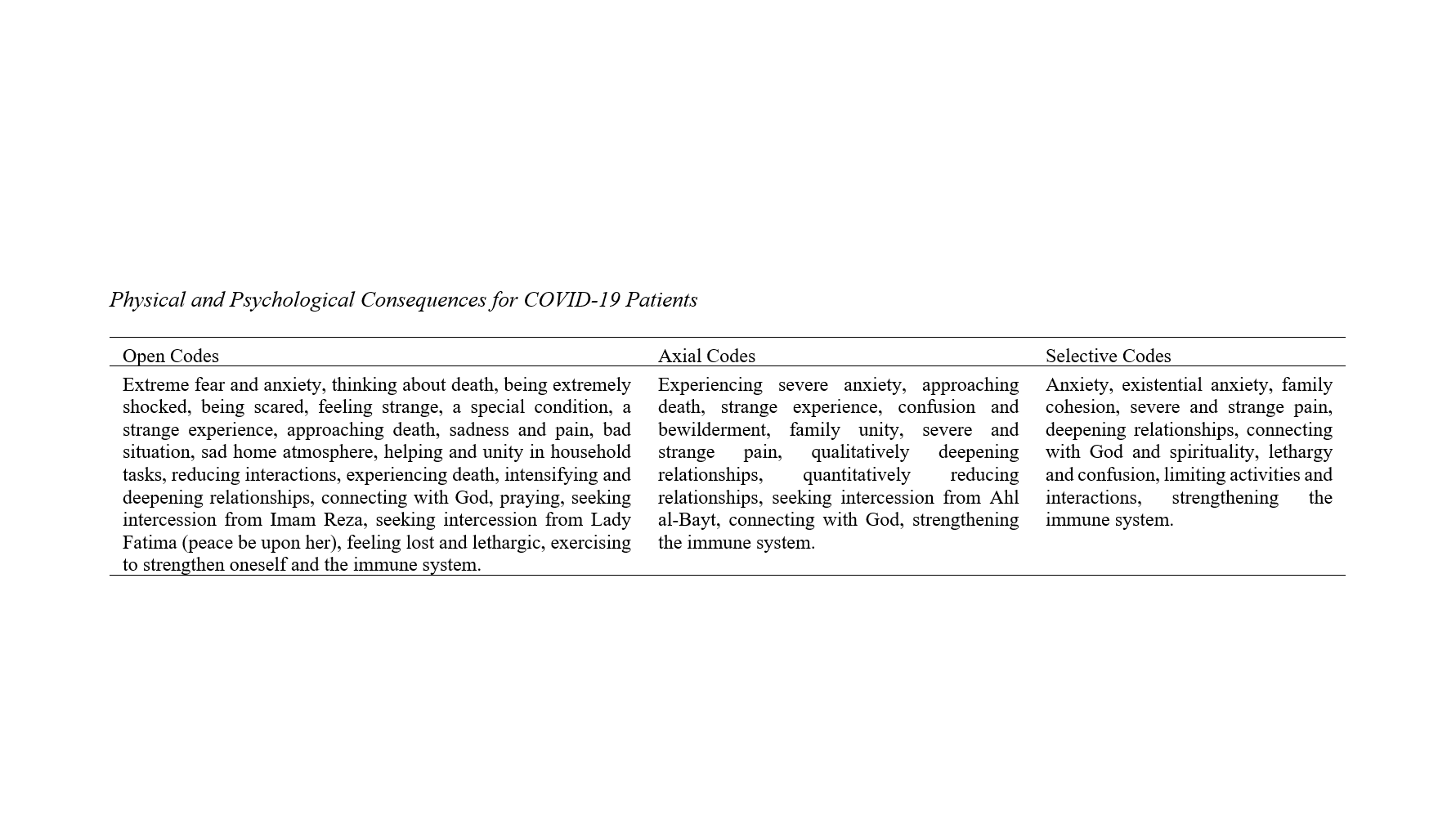
The coronavirus (COVID-19) represents a public health crisis that has imposed numerous restrictions on daily activities. The crisis conditions created by COVID-19 can lead to negative physical and psychological effects on society. In this context, the present study aims to document the physical and psychological consequences of COVID-19 using a qualitative grounded theory approach. This study is applied in its aim and qualitative in nature. The strategy employed in this research is the grounded theory method. The statistical population and sample of this study consisted of 11 individuals infected with COVID-19, who were selected through accessible and purposive sampling due to the nature of the research. This study was conducted using semi-structured interviews with COVID-19 patients until the point of data saturation was reached, and the data obtained from the interviews were subsequently analyzed. Based on the findings, the physical consequences of experiencing COVID-19 included fatigue and lethargy, severe and indescribable pain, an enhanced immune system, and restricted activities. On the other hand, the psychological consequences included experiencing anxiety, family cohesion, existential anxiety (fear of death), strengthened connection with God and spirituality, and deepened relationships. The findings of this study support the notion that every crisis has another side, which includes opportunities that arise during and after the confrontation with the crisis, providing conditions for further growth and development. Therefore, alongside necessary actions and measures such as stress and anxiety management training to prevent the compounded effects of the disease and its associated anxiety, it is also essential to leverage the positive opportunities and outcomes presented by this crisis (COVID-19).
Downloads
References
1. Pastor C. Sentiment Analysis of Filipinos and Effects of Extreme Community Quarantine Due to Coronavirus (COVID-19) Pandemic. SSRN Electronic Journal. 2020. [DOI]
2. Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain, Behavior, and Immunity. 2020;88:916-9. [PMID: 32169498] [PMCID: PMC7102670] [DOI]
3. Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, Gulyaeva AA, et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology. 2020;5(4):536-44. [PMID: 32123347] [PMCID: PMC7095448] [DOI]
4. Farnoosh G, Alishiri G, Hosseini Zijoud SR, Dorostkar R, Jalali Farahani A. Understanding the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus Disease (COVID-19) Based on Available Evidence - A Narrative Review. Journal of Military Medicine. 2022;22(1):1-11. [DOI]
5. Alipour A, Ghadami A, Alipour Z, Abdollahzadeh H. Preliminary validation of the Corona Disease Anxiety Scale (CDAS) in the Iranian sample. Health Psychology. 2020;8(32):163-75. [DOI]
6. Masoudi Sani R, Bahmani B, Asgari A, Khanjani MS, Pakniya N. Construction, validity and reliability of existential anxiety questionnaire (QFEA). Clinical Psychology and Personality. 2020;13(2):151-62.
7. Rahmatinejad P, Yazdi M, Khosravi Z, Shahisadrabadi F. Lived Experience of Patients with Coronavirus (Covid-19): A Phenomenological Study. rph. 2020;14(1):71-86.
8. Lee S. Replication analysis of the Coronavirus Anxiety Scale. Dusunen Adam: The Journal of Psychiatry and Neurological Sciences. 2020;33. [DOI]
9. Yang Y, Lu Q-B, Liu M-J, Wang Y-X, Zhang A-R, Jalali N, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. medRxiv. 2020:2020.02.10.20021675. [DOI]
10. Pfefferbaum B, North Carol S. Mental Health and the Covid-19 Pandemic. New England Journal of Medicine. 2020;383(6):510-2. [PMID: 32283003] [DOI]
11. Zare H, Eisazadeh F. Relationship between Disease Control Perception and Risk Perception with Self- care Behaviors in Patients Discharged from Hospital Due to COVID-19: Path Analysis Study. rph. 2020;14(1):102-14.
12. Corey G. Theory and Practice of Counseling and Psychotherapy: Cengage Learning; 2017.
13. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. Journal of Thrombosis and Haemostasis. 2020;18(6):1421-4. [PMID: 32271988] [PMCID: PMC7262324] [DOI]
Downloads
Additional Files
Published
License
Copyright (c) 2024 Reza Ghaffarzadeh Namazi (Corresponding Author); Aghil Mohseni Rad, Aboalghasem Isamorad (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.