The Effectiveness of a Combined Pelvic Floor Exercise Program and Desensitization-Based Sex Therapy on Pain and Sexual Satisfaction in Female Athletes
Keywords:
pelvic floor muscle training, sex therapy, desensitization, dyspareunia, sexual satisfaction, female athletesAbstract
Objective: This study evaluated the effectiveness of an integrated pelvic floor muscle training program combined with desensitization-based sex therapy on sexual pain and sexual satisfaction in female athletes.
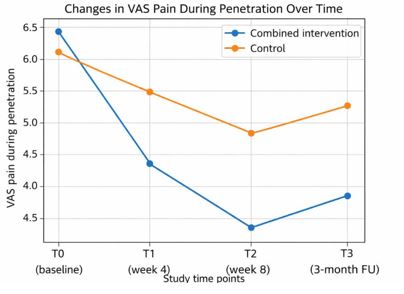
Methods and Materials: In a randomized controlled trial, 68 sexually active female athletes (18–40 years) reporting penetration-related pain were allocated to either a combined intervention group (PFMT plus desensitization-based sex therapy; 8 weekly sessions) or an attention-matched education control group. Outcomes were assessed at baseline, post-intervention (8 weeks), and 3-month follow-up. Primary outcomes included pain during intercourse (Visual Analogue Scale, VAS) and sexual satisfaction (Female Sexual Function Index, FSFI). Secondary outcomes included sexual distress, pain catastrophizing, and pelvic floor muscle strength. Data were analyzed using intention-to-treat mixed-effects models.
Findings: At post-intervention, the combined intervention group demonstrated significantly greater reductions in sexual pain compared with controls (adjusted mean difference = −1.0, 95% CI −1.6 to −0.4; p = .001; Cohen’s d = 0.60). Sexual satisfaction improved significantly in the intervention group (adjusted difference = +3.1 FSFI points, 95% CI 1.4–4.8; p < .001; d = 0.65). Improvements were largely maintained at the 3-month follow-up. Significant reductions were also observed in pain catastrophizing (d = 0.70) and sexual distress (d = 0.72), alongside objective gains in pelvic floor muscle strength (p < .001).
Conclusion: A combined PFMT and desensitization-based sex therapy program is an effective, non-invasive intervention for reducing sexual pain and improving sexual satisfaction in female athletes, supporting a biopsychosocial approach to sexual rehabilitation in sports contexts.
Downloads
References
1. Ghaderi F, Bastani P, Hajebrahimi S, Jafarabadi MA, Berghmans B. Pelvic floor rehabilitation in the treatment of women with dyspareunia: a randomized controlled clinical trial. International Urogynecology Journal. 2019;30(11):1849-55. doi: 10.1007/s00192-019-04019-3.
2. Saus-Ortega C, Sierra-Garcia E, Martínez-Sabater A, Chover-Sierra E, Ballestar-Tarín ML. Effect of pelvic floor muscle training on female sexual function: a systematic review and meta-analysis. Nurs Open. 2023;10:5790-6. doi: 10.1002/nop2.1826.
3. Giagio S, Salvioli S, Pillastrini P, Innocenti T. Sport and pelvic floor dysfunction in male and female athletes: a scoping review. Neurourology and Urodynamics. 2021;40(1):55-64. doi: 10.1002/nau.24564.
4. Borrego-Jimenez PS, Flores-Fraile J, Padilla-Fernández BY, et al. Improvement in quality of life with pelvic floor muscle training and biofeedback in patients with painful bladder syndrome/interstitial cystitis. Journal of Clinical Medicine. 2021;10(4):862. doi: 10.3390/jcm10040862.
5. Gabrielsen R, Tellum T, Bø K, Engh ME, Frawley H, Nedregård Tveito S, et al. Supervised exercise and pelvic floor muscle training eases current pelvic and genital pain but not worst pelvic and genital pain in women with endometriosis: a randomised trial. Journal of Physiotherapy. 2025;71(4):246-53. doi: 10.1016/j.jphys.2025.09.012.
6. Melnik T, Hawton K, McGuire H. Interventions for vaginismus. Cochrane Database of Systematic Reviews. 2012(12):CD001760. doi: 10.1002/14651858.CD001760.pub2.
7. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129-36. doi: 10.1126/science.847460.
8. Pukall CF, Goldstein AT, Bergeron S, Foster D, Stein A, Kellogg-Spadt S, et al. Vulvodynia: definition, prevalence, impact, and pathophysiological factors. Journal of Sex Medicine. 2016;13(3):291-304. doi: 10.1016/j.jsxm.2015.12.021.
9. Thomas HN, Thurston RC. A biopsychosocial approach to women's sexual function and dysfunction at midlife: a narrative review. Maturitas. 2016;87:49-60. doi: 10.1016/j.maturitas.2016.02.009.
10. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews. 2018;2018(10):CD005654. doi: 10.1002/14651858.CD005654.pub4.
11. Morin M, Carroll MS, Bergeron S. Systematic review of the effectiveness of physical therapy modalities in women with provoked vestibulodynia. Sex Medicine Reviews. 2017;5(3):295-322. doi: 10.1016/j.sxmr.2017.02.003.
12. Brotto LA, Zdaniuk B, Chivers ML, Jabs F, Grabovac A, Lalumière ML, et al. A randomized trial comparing group mindfulness-based cognitive therapy with group supportive sex education and therapy for the treatment of female sexual interest/arousal disorder. Journal of Consulting and Clinical Psychology. 2021;89(7):626-39. doi: 10.1037/ccp0000661.
13. Goldstein AT, Pukall CF, Brown C, Bergeron S, Stein A, Kellogg-Spadt S. Vulvodynia: assessment and treatment. Journal of Sex Medicine. 2016;13(4):572-90. doi: 10.1016/j.jsxm.2016.01.020.
14. Bø K, Nygaard IE. Is physical activity good or bad for the female pelvic floor? A narrative review. Sports Medicine. 2020;50(3):471-84. doi: 10.1007/s40279-019-01243-1.
15. Alappattu MJ, Bishop MD. Psychological factors in chronic pelvic pain in women: relevance and application of the fear-avoidance model of pain. Physical Therapy. 2011;91(10):1542-50. doi: 10.2522/ptj.20100368.
16. Vlaeyen JWS, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. 2012;153(6):1144-7. doi: 10.1016/j.pain.2011.12.009.