Comparative Analysis of Physical Activity, Time Management, and Self-Care Among Individuals with Type 2 Diabetes: A Multi-Population Cross-Sectional Study
Keywords:
Diabetes Mellitus Type 2, T2DM, Self-Care, Physical Activity, Time Management, Cultural CharacteristicsAbstract
Objective: The present study aims to examine the relationships among time management, physical activity, and self-care behaviors in individuals with T2DM, with a cross-population comparative method to better understand adherence challenges and inform culturally responsive strategies for diabetes care.
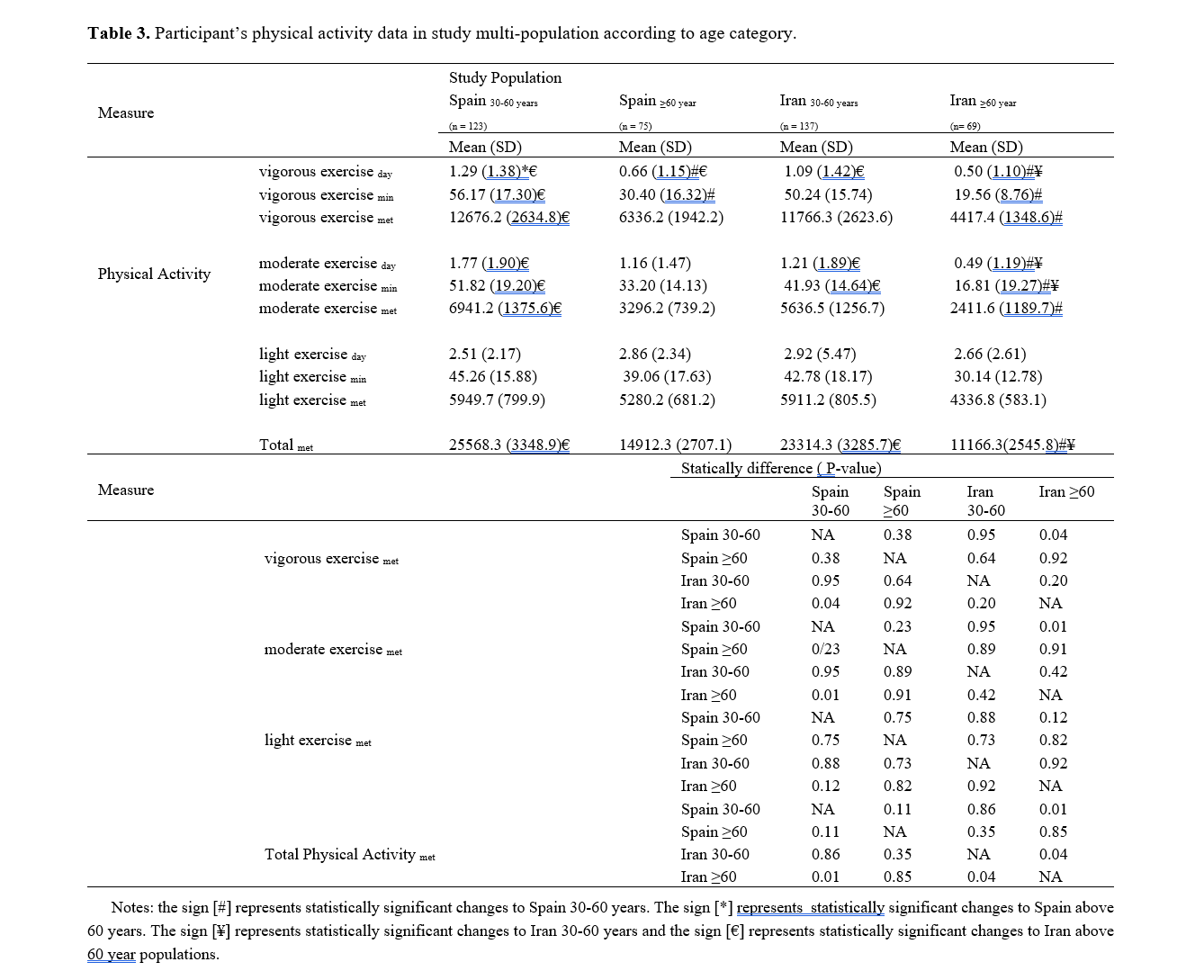
Methods: This cross-sectional descriptive-analytical study examined the relationships between physical activity, time management, and self-care behaviors in adults with type 2 diabetes from Spanish and Iranian populations (n= 404, ). Validated questionnaires—IPAQ-SF, TMBS, and DSMQ—were used to assess physical activity Met, time use, and diabetes-related self-care, respectively, with all data collected ethically under approval code. Statistical analyses included MANOVA, Bonferroni-adjusted post hoc tests, and Pearson correlations to evaluate differences and associations across country, gender, and interaction effects.
Results: Significant differences were found in physical activity and time management across gender, age, and cultural groups, with Spanish males demonstrating higher scores. No group-level differences were observed in self-care behaviors. Time management was positively correlated with both physical activity and self-care in both populations.
Conclusion: This comparative study highlights time management as a key behavioral determinant of self-care in individuals with type 2 diabetes, surpassing physical activity in predictive strength across Spanish and Iranian cohorts. Findings underscore the need for culturally tailored, time-focused interventions that support sustainable self-management, particularly among older adults and women. Culturally tailored strategies—such as Iran’s localized health instruction initiatives and Spain’s region-specific dietary counseling rooted in Mediterranean traditions—play a fundamental role in enhancing diabetes self-management. By connecting clinical objectives with cultural recognition and personal relevance, these suggestions foster greater patient engagement, behavioral adherence, and long-term health improvement.
Downloads
References
1. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239-51. [PMID: 28190580] [DOI]
2. Zhuo X, Zhang P, Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013;45(3):253-61. [PMID: 23953350] [DOI]
3. Qin L, Knol MJ, Corpeleijn E, Stolk RP. Does physical activity modify the risk of obesity for type 2 diabetes: a review of epidemiological data. Eur J Epidemiol. 2010;25(1):5-12. [PMID: 19847656] [PMCID: PMC2807936] [DOI]
4. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065-79. [PMID: 27926890] [PMCID: PMC6908414] [DOI]
5. Umpierre D, Ribeiro PAB, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes. JAMA. 2011;305(17):1790-9. [PMID: 21540423] [DOI]
6. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of Diabetes & Metabolic Disorders. 2013;12(1):14. [PMID: 23497559 ] [PMCID: PMC3599009] [DOI]
7. Al-Khawaldeh OA, Al-Hassan MA, Froelicher ES. Self-care behaviors of Jordanian patients with type 2 diabetes. International Journal of Nursing Practice. 2012;18(3):282-91.
8. Claessens BJ, van Eerde W, Rutte CG, Roe RA. A review of the time management literature. Personnel Review. 2007;36(2):255-76. [DOI]
9. Kumar S, Moseson H, Uppal J, Juusola JL. A diabetes self-management program designed for low-income populations: A randomized controlled trial. Preventing Chronic Disease. 2018;15:E26.
10. Gellert P, Ziegelmann JP, Lippke S, Schwarzer R. Future time perspective and health behaviors: Temporal framing of self-regulatory processes in physical exercise and dietary behaviors. Annals of Behavioral Medicine. 2015;49(5):707-15. [PMID: 22015438]
11. Kocalevent RD, Hinz A, Brähler E. Standardization of a time management scale in the general population. BMC Psychology. 2014;2(1):1-7.
12. Forde C. Scoring the international physical activity questionnaire (IPAQ). 2018.
13. Indreica A, López-Moreno A, Sánchez-Gutiérrez C. Time management, Mediterranean diet adherence, and physical activity among university students. Nutrients. 2022;14(18):3762.
14. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health and quality of life outcomes. 2013;11(1):138. [PMID: 23937988] [PMCID: PMC3751743]
15. Narayanan S, Patel R, Koenig M. Routine matters: Time management, exercise, and mental health in young adults. Journal of Wellness Psychology. 2025;12(1):77-89.
16. Yan Z, Liu Q, Zhang W. Age and activity: Longitudinal links between physical activity intensity and mental health in adolescents. Youth Wellness Quarterly. 2024;9(4):203-14.
17. Altunalan H, Yilmaz Y, Arican G. The impact of physical activity on sleep quality in adults: A cross-sectional study. Journal of Health and Wellness. 2024;19(2):55-64.
18. Bailey JR, Tsai L, Chandra N. Timing matters: Morning exercise and cardiometabolic outcomes in middle-aged adults. Preventive Cardiology Review. 2024;27(3):118-26.
19. Domínguez-Amorós M, Aparicio-Chueca P. Physical activity behaviors across Europe: Motivation vs time availability. European Journal of Sport Studies. 2020;8(1):12-21.
20. Kundakcı H, Gençoğlu C, Demirtaş M. Psychological barriers in physical activity engagement among Turkish university students. Journal of Cultural Health Psychology. 2024;11(2):91-104.
21. Zhang S, Wu J, Chen Y. Motivation and procrastination as predictors of physical activity among college students. Asian Journal of Behavioral Health. 2024;6(1):34-45.
22. Terzi N, Mert E, Topçu B. Leisure satisfaction vs time structure: Impacts on life quality in older adults. International Journal of Aging and Society. 2024;10(3):150-62.
23. Healy S, Kirk A, Vincent R. Reconsidering time constraints in physical activity: Introduction of the EXPERT model. International Journal of Behavioral Medicine. 2024;31(1):47-59.
24. Morris A, Greene T. Interdependent behavioral systems in chronic illness management. Chronic Care Perspectives. 2022;13(2):33-49.
25. Sakai H, Nikkhah S, Tinsley J. Multifaceted models of behavior in chronic illness contexts. Global Chronic Disease Journal. 2023;30(1):17.
26. Liang X, Zane A, McClure H. Identity-focused behavior models and their impact on health adherence. Journal of Health Identity. 2021;11(3):58-70.
27. Tobias A, Nordin K. Emotional drivers of physical activity: Toward a non-clinical understanding of exercise motivation. Behavioral Insights Review. 2022;8(3):92-104.
28. Ellis J, Nguyen R, Jacobs M. Planning and persistence: Time structure and therapeutic engagement among diabetic patients. Health Psychology Frontiers. 2023;21(2):110-24.
29. Foster G, Tang W, Ramirez J. Time planning and diet monitoring: Behavioral predictors in diabetes self-care. Journal of Nutrition & Behavior. 2022;29(1):45-57.
30. Rahmani S, Karimi L, Behnam H. Cultural restrictions and gendered time access: A study in Iranian urban centers. Journal of Sociology and Health. 2023;28(1):72-86.
31. Al-Sabbagh R, El-Deek S. Time inequality and female health behaviors in Middle Eastern urban contexts. Arab Journal of Public Health. 2021;15(1):25-39.
32. Thorne S, Kamal A. Aging and physical activity: A scoping review of barriers in culturally diverse populations. Journal of Gerontology & Health Promotion. 2023;39(4):145-60.
33. Neto JP, Sakamoto R, Lima F. Aging and physical activity disengagement: Institutional and personal barriers. Geriatric Policy Review. 2022;19(3):84-95.
34. Choi H, Menon A. Work-life imbalance and self-care neglect: Findings from busy professionals with diabetes. Occupational Health Insights. 2022;14(1):64-72.
35. DeWitt K, Chen L. Time structure as a stress-buffer in chronic disease: Experimental evidence. Journal of Behavioral Science. 2023;38(3):203-19.
36. Villanueva C, Desai P, Arvidsson L. Emotional regulation and self-management in chronic illness: A transdiagnostic perspective. Journal of Behavioral Medicine. 2022;45(1):58-74.
37. Nasiri N, Bolton P. Affective engagement in habit formation: Rethinking motivation in chronic disease contexts. Emotion and Behavior. 2021;12(4):119-30.
38. Park Y, Shim H, Ghosh S. Digital scheduling and health adherence in diabetic populations: Comparative analytics. Mobile Health Science. 2023;14(2):38-49.
39. Cárdenas E, Hill C. Bridging digital gaps in chronic illness care: Equity strategies for eHealth adoption. Journal of Digital Wellness. 2022;9(4):191-203.
40. Rocha T, Faramarzi S. Behavioral adaptation under cultural constraint: Comparing diabetes management across nations. International Social Health Review. 2021;16(2):141-56.
41. Al-Mutairi A, Hassan Y, Sahab A. Culture-bound health beliefs and diabetes management: A global review. International Journal of Health Psychology. 2022;17(2):88-103.
42. Kim D, Soraya F. Social support networks and behavioral synchrony: A cross-cultural study of health routines. Global Psychology Bulletin. 2022;34(4):102-18.
43. Schwarzer R, Lippke S, Luszczynska A. The Health Action Process Approach revisited: Planning and behavior maintenance in chronic care. Applied Psychology: Health and Well-Being. 2023;15(2):89-108.
44. Lau M, D'Souza S. The Behavioral Cascade Hypothesis: Foundational habits and lifestyle resilience. Behavioral Research Digest. 2022;18(2):89-97.
45. Mukherjee R, Khan F, Badawi A. Behavioral scaffolding in chronic disease prevention: A training model. Applied Health Promotion. 2023;26(1):71-83.
46. Michie S, van Stralen MM, West R. The behavior change wheel: A new method for characterizing and designing behavior change interventions. Implementation Science. 2011;6(1):42. [PMID: 21513547] [PMCID: PMC3096582] [DOI]
47. Sheikholeslami L, Duncan M. Narrative inquiry in health psychology: Capturing lived experience in diabetes. Qualitative Health Research. 2022;32(6):312-26.
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2025 Somayeh Azarian (Author); Marefat Siahkouhian (Corresponding Author); Ana Sofia Alves, Hadi Nobari (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.