Predictive Modeling of Innovation Failure Risk from Organizational Stress, Workload Distribution, and Team Conflict Using Machine Learning Classification
Keywords:
Innovation failure risk, organizational stress, workload distribution, team conflict, machine learning, predictive analytics, organizational behavior, innovation managementAbstract
Objective: The objective of this study was to develop and validate a machine learning–based predictive model for estimating innovation failure risk using organizational stress, workload distribution, and team conflict as primary predictors.
Methods and Materials: This quantitative cross-sectional study was conducted among 612 full-time employees from innovation-driven organizations in Malaysia. Data were collected using standardized survey instruments measuring organizational stress, workload distribution, team conflict, and perceived innovation failure risk. After psychometric validation, the dataset underwent preprocessing including normalization, outlier detection, and feature engineering. Innovation failure risk was converted into a binary classification outcome. Multiple machine learning classifiers were trained and compared, including logistic regression, support vector machines, random forest, gradient boosting, and extreme gradient boosting. Hyperparameter optimization and nested cross-validation were applied to ensure model stability and generalizability.
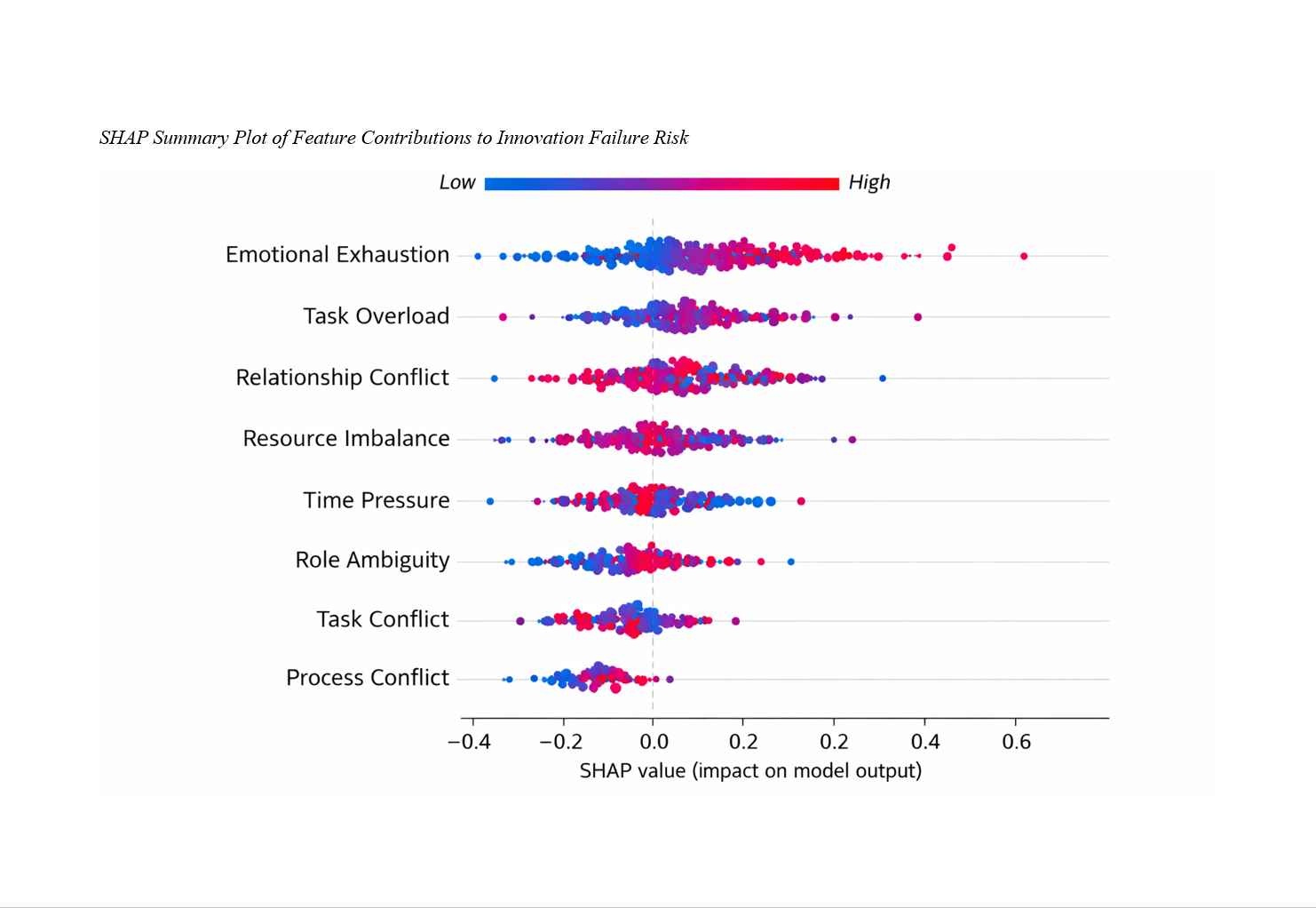
Findings: The XGBoost classifier achieved the highest predictive performance with an accuracy of 94%, precision of 93%, recall of 92%, F1-score of 92%, and AUC of 0.97, significantly outperforming all baseline models. Feature importance analysis revealed that emotional exhaustion and task overload were the strongest predictors of innovation failure risk, followed by relationship conflict and resource imbalance. The final model demonstrated high sensitivity for detecting high-risk innovation cases, confirming the robustness and reliability of the proposed predictive framework.
Conclusion: The findings demonstrate that innovation failure risk is strongly driven by human-centered organizational factors and can be accurately predicted using advanced machine learning models. The proposed framework provides organizations with a powerful early-warning system for preventing innovation breakdowns and strengthening innovation sustainability through proactive management of psychological and structural risk factors.
Downloads
References
Akl, A., Mohiyaldeen, I., Alshatti, R., Alenezi, O., Dougherty, R. J., Al-Raihan, A., Alotaibi, S., Tadros, N., & Longenecker, J. C. (2022). The Prevalence of Burnout and Its Associated Factors Among Surgical Specialists in Kuwait Ministry of Health Hospitals. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.679834
Badheeb, A. M., Almutairi, M. A., Almakrami, A. H., Aman, A. A., Al-Swedan, A. D., Alrajjal, K., Seada, I. A., Bakar, A. A., Alkarak, S., Ahmed, F., Babiker, A., Susheer, S., Badheeb, M., Almutairi, M., & Obied, H. Y. (2024). Factors Affecting Length of Stays in the Emergency Department of a Teaching Hospital: A Retrospective Study From Najran, Saudi Arabia. Cureus. https://doi.org/10.7759/cureus.64684
Barnes, C. M., Wagner, D. T., Schabram, K., & Boncoeur, D. (2022). Human Sustainability and Work: A Meta-Synthesis and New Theoretical Framework. Journal of Management, 49(6), 1965-1996. https://doi.org/10.1177/01492063221131541
Che Mohamad Padali Che, M., Johari, K. S. K., & Mahmud, M. I. (2024). Testing the Healthy School Organisation Instrument (I-Os) and the Holistic Psychological Well-Being Model of School Organisations. International Journal of Learning Teaching and Educational Research, 23(2), 113-144. https://doi.org/10.26803/ijlter.23.2.6
Cildoz, M., Ibarra, A., & Mallor, F. (2023). Acuity-Based Rotational Patient-to-Physician Assignment in an Emergency Department Using Electronic Health Records in Triage. Health Informatics Journal, 29(2). https://doi.org/10.1177/14604582231167430
Coffee, Z. (2025). Trauma-Related Stress and Resilience in a Multistate Sample of Methadone Treatment Staff. Substance Use Research and Treatment, 19. https://doi.org/10.1177/29768357251383239
Devery, K., Winsall, M., & Rawlings, D. (2022). Teams and Continuity of End-of-Life Care in Hospitals: Managing Differences of Opinion. BMJ Open Quality, 11(2), e001724. https://doi.org/10.1136/bmjoq-2021-001724
Dong, F., Huang, W., Chu, C., Lv, L., & Zhang, M. (2023). Influence of Workplace Stress and Social Support on Humanistic Caring Ability in Chinese Nurses. Nursing Open, 10(6), 3603-3612. https://doi.org/10.1002/nop2.1606
Ehmidat, M., Dawabsha, K., Manasrah, A., Salameh, H., Khalili, H., Waleed, S., shanann, S., Abudaia, S., Jaber, M., sarahneh, h., Fakhouri, S., & Mohamed, S. A. (2025). Effect of Burnout Due to Heavy Workload on Surgical Residents: A Multi-National Cross-Sectional Study. https://doi.org/10.21203/rs.3.rs-7101378/v1
García, P., Stephen, P., Shah, S., Smith, M., Jeong, Y., Devon-Sand, A., Tai-Seale, M., Takazawa, K., Clutter, D., Vogt, K., Lugtu, C., Rojo, M., Lin, S., Shanafelt, T. D., Pfeffer, M. A., & Sharp, C. (2024). Artificial Intelligence–Generated Draft Replies to Patient Inbox Messages. JAMA Network Open, 7(3), e243201. https://doi.org/10.1001/jamanetworkopen.2024.3201
Irwan, I. (2024). Workplace Conflict: Its Impact on Employee Motivation and Productivity. Paradoks Jurnal Ilmu Ekonomi, 7(4), 481-494. https://doi.org/10.57178/paradoks.v7i4.993
Kuhns, J. B., Messer, S., & Exum, M. L. (2024). Process Mapping Homicide Investigations and Estimating Resource Requirements for Homicide Units: Findings From a Case Study in the United States. The Police Journal Theory Practice and Principles, 98(1), 197-220. https://doi.org/10.1177/0032258x241258363
Metersky, M. L., Rodrick, D., Ho, S. Y., Galusha, D., Timashenka, A., Grace, E. N., Marshall, D., Eckenrode, S., & Krumholz, H. M. (2024). Hospital COVID-19 Burden and Adverse Event Rates. JAMA Network Open, 7(11), e2442936. https://doi.org/10.1001/jamanetworkopen.2024.42936
Narciso, I., Albuquerque, S., & Nunes, S. (2024). Addiction Interprofessional Experiences of Care: Stress, Coping and Transformation. International journal of mental health nursing, 33(4), 928-936. https://doi.org/10.1111/inm.13289
Ooijen, W. B., Malfait, S., Waal, G. H., & Hafsteinsdøttir, T. B. (2023). Nurses' Motivations to Leave the Nursing Profession: A Qualitative Meta‐aggregation. Journal of Advanced Nursing, 79(12), 4455-4471. https://doi.org/10.1111/jan.15696
Prasad, K., McLoughlin, C., Stillman, M., Poplau, S., Goelz, E., Taylor, S., Nankivil, N., Brown, R., Linzer, M., Cappelucci, K., Barbouche, M., & Sinsky, C. A. (2021). Prevalence and Correlates of Stress and Burnout Among U.S. Healthcare Workers During the COVID-19 Pandemic: A National Cross-Sectional Survey Study. EClinicalMedicine, 35, 100879. https://doi.org/10.1016/j.eclinm.2021.100879
Reguera‐Carrasco, C., Fernández‐García, E., Alvarez, A. N., Jimenez‐García, V. M., Prada‐Rizoto, M., Corral‐Cortés, Á., & Barrientos‐Trigo, S. (2025). Nurse‐Related Complexity of Care Perceived by Critical Care Nurses: A Multicentre Qualitative Study. Nursing in Critical Care, 30(4). https://doi.org/10.1111/nicc.70100
Saputra, M., & Satrya, A. (2024). Burnout and Quality of Work Life on Job Performance: Mediating Role of Job Satisfaction Among Financial Services Employees. Financial Engineering, 2, 313-325. https://doi.org/10.37394/232032.2024.2.29
Shawahna, R., Maqboul, I., Ahmad, O., Al-Issawy, A., & Abed, B. (2022). Prevalence of Burnout Syndrome Among Unmatched Trainees and Residents in Surgical and Nonsurgical Specialties: A Cross-Sectional Study From Different Training Centers in Palestine. BMC Medical Education, 22(1). https://doi.org/10.1186/s12909-022-03386-8
Shih, K. K., Anderson, A. E., Dai, J., Fellman, B., Moraes, A. R. d., Stanton, P., Nelson, C. A., Cruz, V. D., & Bruera, É. (2023). Hybrid Work From Home Clinical Academic Environment: A One-Year Follow-Up Survey of Attitudes and Beliefs of Members of a Department of Palliative Care, Rehabilitation, and Integrative Medicine. Journal of Palliative Medicine, 26(3), 342-352. https://doi.org/10.1089/jpm.2022.0203
Taylor, G. A., Ayyala, R. S., & Coley, B. D. (2022). How Did We Get Here? Thoughts on Health Care System Drivers of Pediatric Radiology Burnout. Pediatric Radiology, 52(6), 1019-1023. https://doi.org/10.1007/s00247-022-05318-6
Wang, D., Hall, M. E. L., Shannonhouse, L., Mize, M. C., Aten, J. D., Davis, E. B., Tongeren, D. R. V., & Annan, K. (2021). Why Humility Is Vital to Effective Humanitarian Aid Leadership: A Review of the Literature. Disasters, 45(4), 797-818. https://doi.org/10.1111/disa.12446
Wolfe, A. H. J., Hinds, P. S., Arnold, R. M., Soghier, L., & Tompkins, R. (2022). Vulnerability of Inexperience: A Qualitative Exploration of Physician Grief and Coping After Impactful Pediatric Patient Deaths. Journal of Palliative Medicine, 25(10), 1476-1483. https://doi.org/10.1089/jpm.2022.0050
Zhao, B., Zhang, Z., & Zhang, M. (2025). Unlocking the Paradox: Exploring the Impact of Management Paradox Thinking on Corporate Innovation Performance. Sage Open, 15(3). https://doi.org/10.1177/21582440251359078