Cognitive Avoidance as a Mediator Between Trauma Exposure and Emotional Numbing
Keywords:
trauma exposure, cognitive avoidance, emotional numbingAbstract
Objective: This study aimed to examine the mediating role of cognitive avoidance in the relationship between trauma exposure and emotional numbing among young adults.
Methods and Materials: The research followed a descriptive correlational design using a sample of 445 participants from Greece, selected based on Morgan and Krejcie's sample size table. Data were collected using three standardized instruments: the Life Events Checklist for DSM-5 (LEC-5) for trauma exposure, the Cognitive Avoidance Questionnaire (CAQ) for cognitive avoidance, and the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) for emotional numbing. Descriptive statistics and Pearson correlation coefficients were computed using SPSS-27. Structural Equation Modeling (SEM) was conducted through AMOS-21 to evaluate the mediating effect of cognitive avoidance and the overall fit of the hypothesized model.
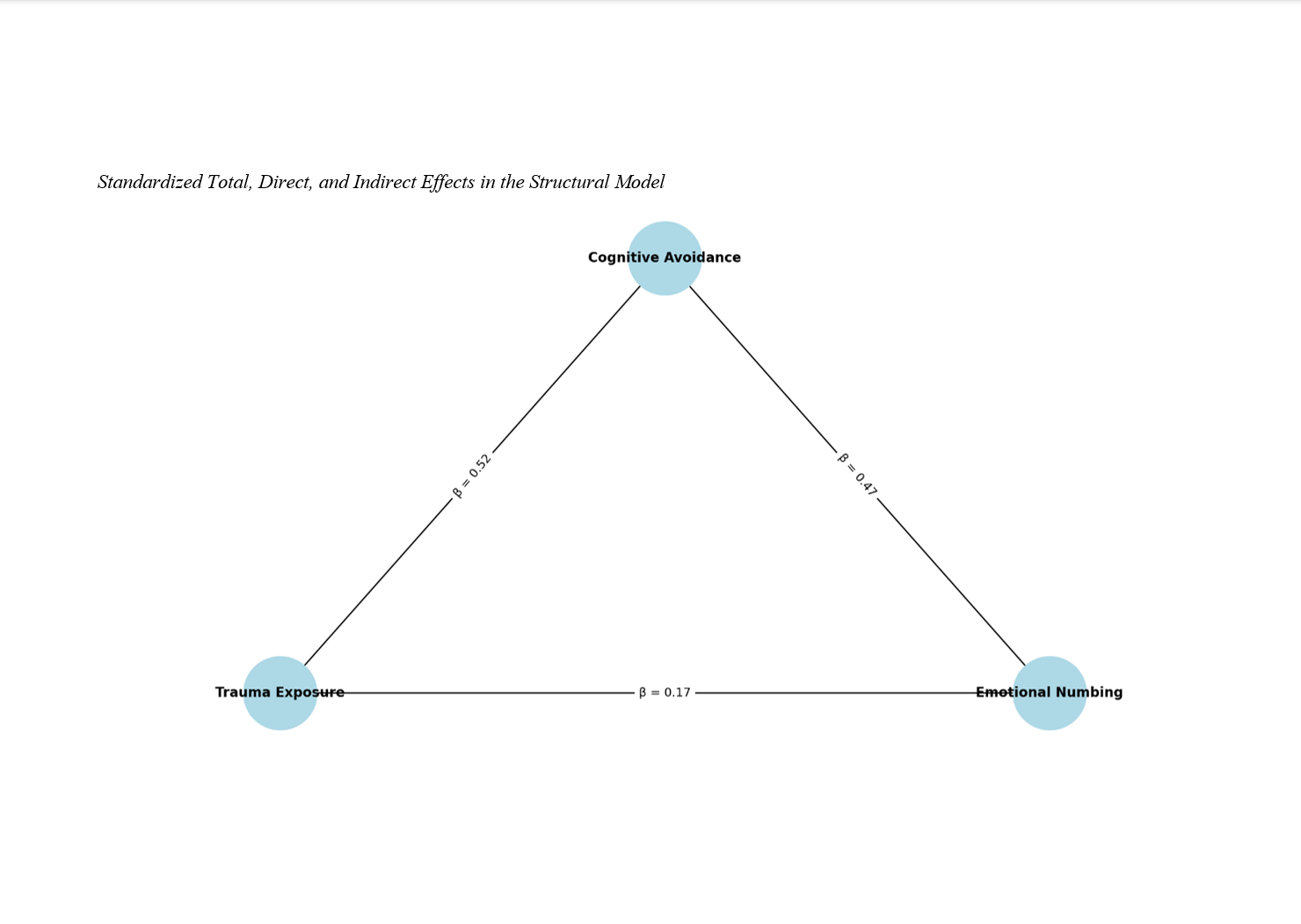
Findings: Participants reported moderate levels of trauma exposure (M = 7.83, SD = 2.61), high cognitive avoidance (M = 78.42, SD = 11.97), and moderate emotional numbing (M = 6.14, SD = 1.72). Pearson correlations indicated significant positive associations between trauma exposure and cognitive avoidance (r = .52, p < .001), trauma exposure and emotional numbing (r = .46, p < .001), and cognitive avoidance and emotional numbing (r = .58, p < .001). The SEM analysis confirmed that cognitive avoidance partially mediated the relationship between trauma exposure and emotional numbing. The model demonstrated good fit indices (χ²/df = 2.07, CFI = 0.96, RMSEA = 0.049). Direct, indirect, and total effects were all statistically significant (p < .01), supporting the hypothesized mediation.
Conclusion: These findings highlight the importance of addressing cognitive avoidance in therapeutic interventions aimed at reducing emotional disengagement in trauma-exposed individuals, particularly in emerging adult populations.
Downloads
References
Ali, A. M., Al‐Amer, R., Kunugi, H., Stănculescu, E., Taha, S. M., Saleh, M., Alkhamees, A. A., & Hendawy, A. O. (2022). The Arabic Version of the Impact of Event Scale-Revised: Psychometric Evaluation Among Psychiatric Patients and the General Public Within the Context of COVID-19 Outbreak and Quarantine as Collective Traumatic Events. Journal of Personalized Medicine, 12(5), 681. https://doi.org/10.3390/jpm12050681
Bakhshaie, J., Zvolensky, M. J., Allan, N. P., Vujanovic, A. A., & Schmidt, N. B. (2015). Differential Effects of Anxiety Sensitivity Components in the Relation Between Emotional Non-Acceptance and Post-Traumatic Stress Symptoms Among Trauma-Exposed Treatment-Seeking Smokers. Cognitive behaviour therapy, 44(3), 175-189. https://doi.org/10.1080/16506073.2015.1004191
Belevegka, A., & Smyth, N. (2024). An Investigation Into the Relationship Between Stress Mindset and Stress Responses: The Role of Coping Mechanisms. Psychology the Journal of the Hellenic Psychological Society, 29(2), 349-366. https://doi.org/10.12681/psy_hps.39610
Bhalla, A., Bamer, A. M., Temes, C. M., Roaten, K., Carrougher, G. J., Schneider, J. C., Stoddard, F. J., Stewart, B. T., Gibran, N. S., & Wiechman, S. A. (2022). Posttraumatic Stress Disorder Symptom Clusters as Predictors of Pain Interference in Burn Survivors: A Burn Model System National Database Study. Journal of Burn Care & Research, 44(1), 27-34. https://doi.org/10.1093/jbcr/irac088
Brody, D. L. (2019). Post-Traumatic Stress Disorder. 86-93. https://doi.org/10.1093/med/9780190054793.003.0012
Carper, T. L. M., Mills, M. A., Steenkamp, M. M., Nickerson, A., Salters‐Pedneault, K., & Litz, B. T. (2015). Early PTSD Symptom Sub-Clusters Predicting Chronic Posttraumatic Stress Following Sexual Assault. Psychological Trauma Theory Research Practice and Policy, 7(5), 442-447. https://doi.org/10.1037/tra0000060
Dixon De Silva, L. E., Ponting, C., Rapp, A. M., Escovar, E., & Chavira, D. A. (2020). Trauma Exposure and Mental Health Symptoms in Rural Latinx Adolescents: The Role of Family Processes. Child Psychiatry & Human Development, 51(6), 934-942. https://doi.org/10.1007/s10578-020-00971-0
Duffy, M., & Wild, J. (2017). A Cognitive Approach to Persistent Complex Bereavement Disorder (PCBD). The Cognitive Behaviour Therapist, 10. https://doi.org/10.1017/s1754470x17000034
Eichhorn, S., Brähler, E., Franz, M., Friedrich, M., & Glaesmer, H. (2014). Traumatic Experiences, Alexithymia, and Posttraumatic Symptomatology: A Cross-Sectional Population-Based Study in Germany. European Journal of Psychotraumatology, 5(1). https://doi.org/10.3402/ejpt.v5.23870
Eth, S., & Pynoos, R. S. (2017). Posttraumatic Stress Disorder in Children. https://doi.org/10.4135/9781483369532.n385
Galano, M. M., Miller, L. E., & Graham‐Bermann, S. A. (2014). Avoidance Symptom Presentation of Preschoolers Exposed to Intimate Partner Violence in a Group Therapy Setting. Child Care in Practice, 20(4), 399-414. https://doi.org/10.1080/13575279.2014.905455
Goldstein, B., Bradley, B., Ressler, K. J., & Powers, A. (2016). Associations Between Posttraumatic Stress Disorder, Emotion Dysregulation, and Alcohol Dependence Symptoms Among Inner City Females. Journal of Clinical Psychology, 73(3), 319-330. https://doi.org/10.1002/jclp.22332
Hardy, A., O’Driscoll, C., Steel, C., Gaag, M. v. d., & Berg, D. V. D. (2020). A Network Analysis of Post-Traumatic Stress and Psychosis Symptoms. Psychological medicine, 51(14), 2485-2492. https://doi.org/10.1017/s0033291720001300
Hecker, T., Ainamani, H. E., Hermenau, K., Haefele, E., & Elbert, T. (2017). Exploring the Potential Distinction Between Continuous Traumatic Stress and Posttraumatic Stress in an East African Refugee Sample. Clinical Psychological Science, 5(6), 964-973. https://doi.org/10.1177/2167702617717023
Kerig, P. K., Bennett, D. C., Thompson, M., & Becker, S. P. (2012). “Nothing Really Matters”: Emotional Numbing as a Link Between Trauma Exposure and Callousness in Delinquent Youth. Journal of Traumatic Stress, 25(3), 272-279. https://doi.org/10.1002/jts.21700
Kim, S.-J., & Sung-pil, Y. (2018). The Influence of Posttraumatic Stress on Suicidal Ideation in Firefighters : Cognitive Emotion Regulation as a Moderator. Fire Science and Engineering, 32(2), 92-101. https://doi.org/10.7731/kifse.2018.32.2.092
Li, G., Hampel, A., Li, C., & Hall, B. J. (2023). Emotional Numbing: A Key Construct in the Assessment of Mental Health During COVID-19 Pandemic. Journal of Pacific Rim Psychology, 17. https://doi.org/10.1177/18344909231217649
Mason, S. M., Flint, A. J., Roberts, A. L., Agnew-Blais, J., Koenen, K. C., & Rich-Edwards, J. W. (2014). Posttraumatic stress disorder symptoms and food addiction in women by timing and type of trauma exposure. JAMA Psychiatry, 71(11), 1271-1278. https://jamanetwork.com/journals/jamapsychiatry/article-abstract/1904804
McLaughlin, K. A., Colich, N. L., Rodman, A. M., & Weissman, D. G. (2020). Mechanisms Linking Childhood Trauma Exposure and Psychopathology: A Transdiagnostic Model of Risk and Resilience. BMC Medicine. https://doi.org/10.1186/s12916-020-01561-6
Mohammd, S., Asgari, Parviz, Makvandi, Behnam, Naderi, Farah. (2022). The Effect of Schema Therapy on Cognitive Avoidance, Anxiety, and Empathy in Couples Referring to Ahvaz Counseling Centers. Family and Health, 11(4), 58-69. https://journal.astara.ir/article_252836.html?lang=en
Post, M., Hanten, G., Li, X., Schmidt, A., Avci, G., Wilde, E. A., & McCauley, S. R. (2014). Dimensions of Trauma and Specific Symptoms of Complex Posttraumatic Stress Disorder in Inner-City Youth: A Preliminary Study. Violence and Victims, 29(2), 262-279. https://doi.org/10.1891/0886-6708.vv-d-12-00097r1
Procaccia, R., & Castiglioni, M. (2022). The Mediating Effect of Cognitive and Emotional Processing on PTSD and Depression Symptoms Reduction in Women Victims of IPV. Frontiers in psychology, 13. https://doi.org/10.3389/fpsyg.2022.1071477
Reddy, M. K., Anderson, B. J., Liebschutz, J. M., & Stein, M. D. (2013). Factor Structure of PTSD Symptoms in Opioid-Dependent Patients Rating Their Overall Trauma History. Drug and Alcohol Dependence, 132(3), 597-602. https://doi.org/10.1016/j.drugalcdep.2013.04.009
Scotta, A. V., Cortez, M. V., & Miranda, A. R. (2022). Insomnia is associated with worry, cognitive avoidance and low academic engagement in Argentinian university students during the COVID-19 social isolation. Psychology, Health & Medicine, 27(1), 199-214. https://doi.org/10.1080/13548506.2020.1869796
Shahini, M., Ghorbaninezhad, M., Kamkar, M., & Naimabady, Z. (2023). The effectiveness of mindfulness-based cognitive therapy on autobiographical memories, cognitive avoidance and cognitive emotion regulation in patients with major depression [Research]. Journal of nursing education, 11(3), 82-93. https://doi.org/10.22034/ijpn.11.3.9
Sippel, L. M., Watkins, L. E., Pietrzak, R. H., Hoff, R. A., & Harpaz‐Rotem, I. (2018). The Unique Roles of Emotional Numbing and Arousal Symptoms in Relation to Social Connectedness Among Military Veterans in Residential Treatment for PTSD. Psychiatry, 81(3), 271-282. https://doi.org/10.1080/00332747.2017.1395313
Solberg, Ø., Birkeland, M. S., Blix, I., Hansen, M. B., & Heir, T. (2016). Towards an Exposure-Dependent Model of Post-Traumatic Stress: Longitudinal Course of Post-Traumatic Stress Symptomatology and Functional Impairment After the 2011 Oslo Bombing. Psychological medicine, 46(15), 3241-3254. https://doi.org/10.1017/s0033291716001860
Thompson‐Hollands, J., Jun, J. J., & Sloan, D. M. (2017). The Association Between Peritraumatic Dissociation and PTSD Symptoms: The Mediating Role of Negative Beliefs About the Self. Journal of Traumatic Stress, 30(2), 190-194. https://doi.org/10.1002/jts.22179
Vanderheyden, W. M., Poe, G. R., & Liberzon, I. (2014). Trauma Exposure and Sleep: Using a Rodent Model to Understand Sleep Function in PTSD. Experimental Brain Research, 232(5), 1575-1584. https://doi.org/10.1007/s00221-014-3890-4
Whitaker, A. M., & Gilpin, N. W. (2016). Inhibition of ERK Phosphorylation Decreases Post‐stress Avoidance in High Stress Reactive Rats. The FASEB Journal, 30(S1). https://doi.org/10.1096/fasebj.30.1_supplement.1231.3
Xue, M., Yuan, Y., Chen, H., Liu, Y., Dai, M., Sun, H., Qu, J., Zhou, T., Zhou, J., Qu, J., Bu, Y., Ji, S., Hu, Y., Yao, Z., Feng, Y., & Gu, X. (2022). Perceived Stress and Symptoms of Post-Traumatic Stress Disorder in Nurses: A Moderated Mediation Model of Maladaptive Cognitive Emotional Regulation and Psychological Capital. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.902558
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.