Impact of a Digital Detox Program on Screen Time and Sleep Hygiene in Adolescents
Keywords:
Digital detox, Screen time, Sleep hygiene, Adolescents, Randomized controlled trial, Behavioral intervention, ChinaAbstract
Objective: This study aimed to assess the effectiveness of a structured digital detox program in reducing screen time and improving sleep hygiene among Chinese adolescents.
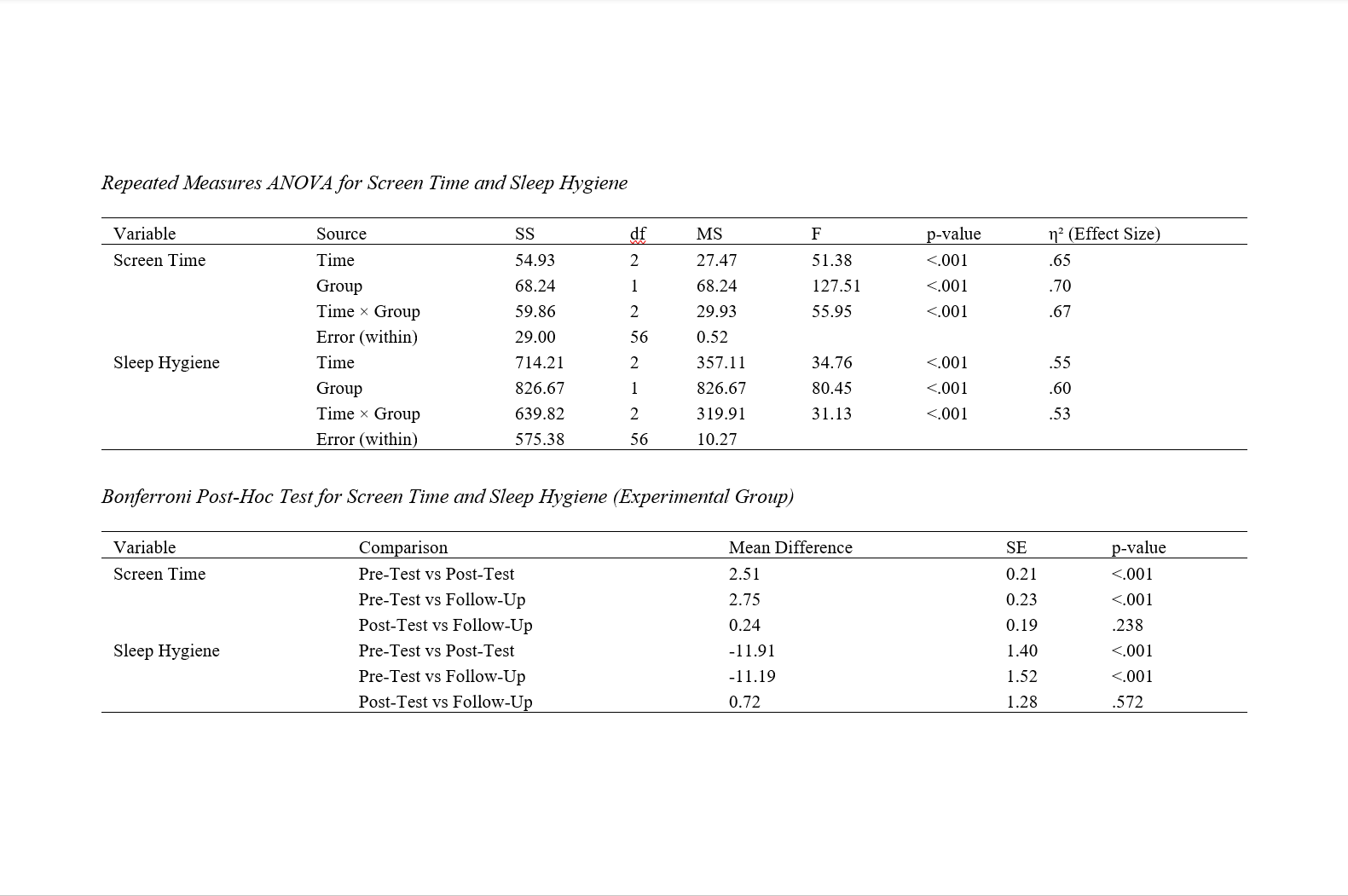
Methods and Materials: Thirty adolescents (aged 13–17) were recruited and randomly assigned to an experimental (n = 15) or control (n = 15) group. Over ten weekly sessions, the experimental group participated in a digital detox intervention featuring psychoeducation, cognitive-behavioral techniques, and goal-setting to minimize excessive screen use. Sleep hygiene education was incorporated through discussions on bedtime routines and reducing nighttime device exposure. The control group received no intervention. Data were collected at three time points: pre-intervention, post-intervention, and a five-month follow-up. Outcomes included self-reported measures of daily screen time and sleep hygiene scores. Repeated measures analysis of variance was conducted to evaluate within- and between-group changes, and Bonferroni post-hoc tests were applied to identify significant pairwise differences.
Findings: The experimental group demonstrated a notable decline in mean daily screen time, from 6.82 hours (SD = 0.76) at baseline to 4.31 hours (SD = 0.65) post-intervention, which remained stable at 4.07 hours (SD = 0.61) at follow-up. Sleep hygiene scores improved significantly, rising from a baseline of 81.27 (SD = 6.24) to 93.18 (SD = 5.77) post-intervention and stabilizing at 92.46 (SD = 5.51) at follow-up. In contrast, the control group showed minimal changes across these time points. Statistical analyses confirmed significant time × group interactions for both variables (p < .001).
Conclusion: Incorporating structured sessions, behavioral monitoring, and sleep education may contribute to healthier technology habits and better sleep practices in this population.
Downloads
References
Alijanzadeh, M., Yahaghi, R., Rahmani, J., Yazdi, N., Jafari, E., Alijani, H., Zamani, N., Fotuhi, R., Taherkhani, E., Buchali, Z., Zarenejad, M., Mahmoudi, N., Shahmahdi, N., Poorzolfaghar, L., Ahmadizade, S., Shahbazkhania, A., Gozal, D., Lin, C. Y., & Pakpour, A. H. (2023). Sleep Hygiene Behaviours Mediate the Association Between Health/E‐health Literacy and Mental Wellbeing. Health Expectations, 26(6), 2349-2360. https://doi.org/10.1111/hex.13837
Arnardóttir, E. S., & Cunningham, J. (2023). Sleep Medicine in Iceland – The Challenges of a Subarctic Small Nation. 360-373. https://doi.org/10.2174/9789815049367123010029
Azzahrah, F. (2025). The Relationship Between Smartphone Use and Sleep Quality in Adolescents. Ahmar Metastasis Health Journal, 4(4), 179-187. https://doi.org/10.53770/amhj.v4i4.450
Beluli, A. (2023). Machine Learning-Based Prediction Model for the Measurement of Mobile Addiction. 56-66. https://doi.org/10.4018/978-1-6684-8582-8.ch004
Bolshakova, S. E., Мадаева, И. М., Berdina, O. N., Храмова, Е. Е., Бугун, О. В., & Рычкова, Л. В. (2024). Prevalence of Sleep Disorders in Teenage Girls in Irkutsk (Questionnaire Data). Acta Biomedica Scientifica, 8(6), 186-193. https://doi.org/10.29413/abs.2023-8.6.18
Chehri, A., Shetabi, M., Khazaie, H., & Zakiei, A. (2023). Sleep Hygiene and Sleep Quality in Iranian Adolescents During the COVID-19 Pandemic. BMC psychology, 11(1). https://doi.org/10.1186/s40359-023-01165-8
Coel, R. A., Pujalte, G. G., Applewhite, A. I., Zaslow, T., Cooper, G., Ton, A., & Benjamin, H. J. (2022). Sleep and the Young Athlete. Sports Health a Multidisciplinary Approach, 15(4), 537-546. https://doi.org/10.1177/19417381221108732
D., S. K., & R., L. (2023). Teenagers Sleeping Pattern Affecting Their Health. International Journal for Multidisciplinary Research, 5(6). https://doi.org/10.36948/ijfmr.2023.v05i06.10841
Dzierzewski, J. M., Nielson, S., & Lopos, J. (2024). 0944 National Sleep Foundation’s 2024 Sleep in America Poll: Sleep Health and Depressive Symptoms in Teenagers. Sleep, 47(Supplement_1), A405-A405. https://doi.org/10.1093/sleep/zsae067.0944
G, C. S., Haarika, V., Tumati, K. R., & Ramisetty, U. M. (2024). The Impact of Screen Time on Sleep Patterns in School-Aged Children: A Cross-Sectional Analysis. Cureus. https://doi.org/10.7759/cureus.55229
Hale, L., & Dzierzewski, J. M. (2024). Screens and Sleep Health—It’s Almost Bedtime, Time to Put Your Phone Away. JAMA Pediatrics, 178(10), 963. https://doi.org/10.1001/jamapediatrics.2024.2757
Hale, L., Hartstein, L. E., Robbins, R., Grandner, M. A., LeBourgeois, M. K., Garrison, M. M., & Czeisler, C. A. (2024). What Do We Know About the Link Between Screens and Sleep Health? , 101-107. https://doi.org/10.1007/978-3-031-69362-5_14
Huang, X., Lin, X., & Yang, H. (2023). Exploration of the Association Between Sleep Quality and Dietary Nutrition in Adolescents/Research Advances. Highlights in Science Engineering and Technology, 80, 502-509. https://doi.org/10.54097/stf91d64
Kushwaha, U., Khadgi, S., Kafle, S., & Khadgi, S. (2024). Technology on Sleeping Patterns of Youths. NPRC J. Multidis. Res., 1(9), 125-134. https://doi.org/10.3126/nprcjmr.v1i9.74169
Lee, J., & Cho, A. (2023). Blue Light Blocking Glasses: Do They Do What They Promise? J Emerg Invest. https://doi.org/10.59720/23-028
Maulida, L., Selviana, S., & Nuzula, F. (2024). Tiktok Social Media Addiction With Bedtime Procrastination. International Journal of Advanced Health Science and Technology, 4(1). https://doi.org/10.35882/ijahst.v4i1.312
Muslimah, P. A., & Khotimah, S. (2022). Influence Schroth Exercise on Decreasing the Degree of Scoliosis in Teenagers :Narrative Review. Sport and Fitness Journal, 10(3), 172. https://doi.org/10.24843/spj.2022.v10.i03.p01
Nagata, J. M., Chu, J., Ganson, K. T., Murray, S. B., Iyer, P., Gabriel, K. P., Garber, A. K., Bibbins-Domingo, K., & Baker, F. C. (2023). Contemporary screen time modalities and disruptive behavior disorders in children: a prospective cohort study. Journal of Child Psychology and Psychiatry, 64(1), 125-135. https://doi.org/10.1111/jcpp.13673
Nguyen, A., Chaung, M., & Valenzuela, A. (2024). 1159 the Cyclical Daytime Sleeper: A Rare Case of a Sighted Teenager With Non-24-Hour Sleep-Wake Disorder. Sleep, 47(Supplement_1), A496-A497. https://doi.org/10.1093/sleep/zsae067.01159
Pchelina, P., Sursaev, V. A., & Полуэктов, М. Г. (2022). Information Overload and Sleep Disorders. Meditsinskiy Sovet = Medical Council(11), 54-60. https://doi.org/10.21518/2079-701x-2022-16-11-54-60
Richards, A., & Gutter, A. (2023). A Review of the Effects of Social Media on Sleep in High-School-Aged Students. Journal of Student Research, 12(3). https://doi.org/10.47611/jsrhs.v12i3.4957
Rowland, T. (2023). Circadian Rhythms, Sleep, and the Youth Athlete. 547-C539P137. https://doi.org/10.1093/med/9780192843968.003.0039
Saeed, H., Dwivedi, M., Singh, S., Nandy, A., & Dwivedi, M. (2024). Irregular Sleeping Patterns in Adolescents. 95-106. https://doi.org/10.2174/9789815274400124010009
Samintharapunya, P., & Choksamut, P. (2023). A Literature Review on Sleep Deprivation Among Teenagers Aged 13 to 18. https://doi.org/10.31219/osf.io/wjn2k
Schouwenaars, I. (2023a). A School-Based Sleep Intervention for Autistic Teenagers: Effects on Sleep Quality and Daytime Functioning. https://doi.org/10.31234/osf.io/dz5uf
Schouwenaars, I. (2023b). Sleep and Daytime Functioning in Autistic Teenagers: A Psychological Network Approach. https://doi.org/10.31234/osf.io/sgvz2
Toprak, T., & Karan, M. (2022). Effects of Sleep Deprivation and Early School Start Times on Adolescent Health. Journal of Student Research, 11(3). https://doi.org/10.47611/jsrhs.v11i3.3590
Wickham, S., Brosnan, B., Haszard, J. J., Meredith‐Jones, K., Galland, B. C., & Taylor, R. W. (2024). O002 Sleepy Teens and the Use of Screens: A Repeated Measures Analysis Examining the Relationship Between Pre-Bedtime Screen Use and Sleep. Sleep Advances, 5(Supplement_1), A2-A2. https://doi.org/10.1093/sleepadvances/zpae070.002
Xu, J., Duan, H., Qin, K., & Liu, B. (2024). Association of Screen Time and Mental Disorders Among Chinese Adolescents. https://doi.org/10.21203/rs.3.rs-4233571/v1
Zain, M. A., & Hanif, M. I. (2023). Optimalisasi Manajemen Waktu Tidur Demi Meningkatkan Produktivitas Remaja Dengan Pendekatan Kesehatan Dan Nilai-Nilai Islam. Jubima, 1(4), 153-161. https://doi.org/10.55606/jubima.v1i4.2258
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.