The Mediating Role of Anxiety in the Relationship Between Physical Activity and Premenstrual Syndrome in Female Students
Keywords:
physical activity, anxiety, premenstrual syndrome, female studentsAbstract
Objective: The aim of the present study was to investigate the mediating role of anxiety in the relationship between physical activity and symptoms of premenstrual syndrome among female students.
Methods and Materials: This study was conducted using a descriptive–analytical design. The statistical population consisted of all female students of Islamic Azad University, Shahroud Branch, in the academic year 2023–2024, from whom 145 individuals were selected through convenience sampling. The instruments used included the International Physical Activity Questionnaire (IPAQ), the Beck Anxiety Inventory (BAI), and the Premenstrual Symptoms Screening Tool (PSST). Data were analyzed using linear regression, path analysis, and bootstrapping.
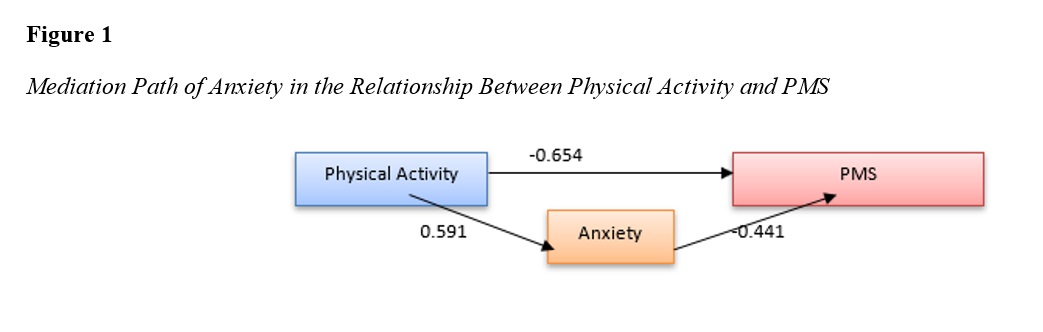
Findings: The results showed that there was a significant negative relationship between physical activity and the severity of premenstrual syndrome symptoms (β = -0.654, p < 0.001); that is, with an increase in physical activity levels, the severity of the syndrome’s symptoms decreased. In addition, anxiety was also found to be a significant negative predictor of premenstrual syndrome symptoms (β = -0.441, p < 0.001), indicating that lower anxiety levels were associated with reduced syndrome symptoms. Furthermore, physical activity was positively and significantly associated with the reverse anxiety score (indicating an actual reduction in anxiety) (β = 0.591, p < 0.001). Path analysis confirmed the partial mediating role of anxiety in the relationship between physical activity and premenstrual syndrome, with the indirect path effect being β = -0.260, which was statistically significant.
Conclusion: Overall, the findings indicated that increasing physical activity can reduce the severity of premenstrual syndrome symptoms both directly and indirectly through reducing anxiety, thereby contributing to the improvement of women’s psychosomatic well-being.
Downloads
References
Amasha, H. A., Mohamed, R. A., & Nageeb, H. (2017). Complementary and alternative therapies for premenstrual syndrome: an exploratory study. Khartoum Medical Journal, 10(3). https://doi.org/10.53332/kmj.v10i3.668
American College of, O., & Gynecologists. (2023). Management of premenstrual disorders. ACOG Clinical Practice Guideline No. 4. https://www.acog.org
Andrade, C. (2016). Premenstrual dysphoric disorder: General overview, treatment strategies, and focus on sertraline for symptom-onset dosing. Indian Journal of Psychiatry, 58(3), 329-331. https://doi.org/10.4103/0019-5545.192014
Bosman, R. C., Jung, S. E., Miloserdov, K., Schoevers, R. A., & aan het Rot, M. (2016). Daily symptom ratings for studying premenstrual dysphoric disorder: A review. Journal of affective disorders, 189, 43-53. https://doi.org/10.1016/j.jad.2015.08.063
Chen, Y., Zhang, X., & Zhang, Y. (2023). Non-pharmacological management of premenstrual syndrome: A review. Frontiers in Public Health, 11, 1111220. https://doi.org/10.3389/fpubh.2023.1111220
Dashti, A., Zargar, Y., & Davoodi, A. (2023). The relationship between mindfulness, self-silencing, difficulties in emotion regulation, and perceived stress with premenstrual syndrome: The mediating role of perceived stress. Quarterly Journal of Clinical Psychology Research, 15(1), 43-56. https://civilica.com/doc/1756325
Dózsa-Juhász, O., Makai, A., Prémusz, V., Ács, P., & Hock, M. (2023). Investigation of premenstrual syndrome in connection with physical activity, perceived stress level, and mental status: A cross-sectional study. Frontiers in Public Health, 11, 1223787. https://doi.org/10.3389/fpubh.2023.1223787
Gharibi, L., Mousavi, S. M., & Bakhshandeh Naneh Karan, M. (2023). Modeling premenstrual syndrome symptoms based on perceived stress with the mediating role of sleep quality among university students. Quarterly Journal of Psychological Growth Research, 12(11), 1-12. https://frooyesh.ir/article-1-4721-fa.html
Gnanasambanthan, S., & Datta, S. (2019). Premenstrual syndrome. Obstetrics, Gynaecology & Reproductive Medicine, 29(10), 281-285. https://doi.org/10.1016/j.ogrm.2019.06.003
Hofmeister, S., & Bodden, S. (2016). Premenstrual syndrome and premenstrual dysphoric disorder. American family physician, 94(3), 236-240. https://pubmed.ncbi.nlm.nih.gov/27479626/
Maleki-Saghooni, N., Karimi, F. Z., Moghadam, Z. B., & Najmabadi, K. M. (2018). The effectiveness and safety of Iranian herbal medicines for treatment of premenstrual syndrome: A systematic review. Avicenna Journal of Phytomedicine, 8(2), 96-113. https://pmc.ncbi.nlm.nih.gov/articles/PMC5885324/
Pearce, E., Jolly, K., Jones, L. L., Matthewman, G., Zanganeh, M., & Daley, A. (2020). Exercise for premenstrual syndrome: a systematic review and meta-analysis of randomised controlled trials. BJGP open, 4(3). https://doi.org/10.3399/bjgpopen20X101032
Pourhaghighi, F., Babalu, M., Izadi, M., & Ebrahimi, S. (2024). Examining the effect of physical activity on primary dysmenorrhea, stress, and cortisol levels in adolescent girls. Proceedings of the 2nd National Conference on Novel Achievements in Physical Education, Sports Sciences, and Psychology, University of Mazandaran,
Ranjbaran, M., Omani Samani, R., Almasi-Hashiani, A., Matourypour, P., & Moini, A. (2017). Prevalence of premenstrual syndrome in Iran: A systematic review and meta-analysis. International Journal of Reproductive BioMedicine, 15(11), 679-686. https://doi.org/10.29252/ijrm.15.11.679
Rassolnia, A., & Nobari, H. (2024). The Impact of Socio-Economic Status and Physical Activity on Psychological Well-being and Sleep Quality Among College Students During the COVID-19 Pandemic. International Journal of Sport Studies for Health, 7(2), 1-12. https://doi.org/10.61838/kman.intjssh.7.2.1
Rosner, J., Samardzic, T., & Sarao, M. S. (2019). Physiology, female reproduction. https://www.ncbi.nlm.nih.gov/books/NBK537132/
Saki, M., Akbari, S., Saki, M., Tarrahi, M. J., Gholami, M., & Pirdadeh, S. (2015). The effect of primrose oil on the premenstrual syndrome among the female students in Lorestan University of Medical Sciences: A triple blind study. Journal of Nursing and Midwifery Sciences, 2(1), 20-26. https://doi.org/10.4103/2345-5756.231415
Shi, Y., Shi, M., Liu, C., Sui, L., Zhao, Y., & Fan, X. (2023). Associations with physical activity, sedentary behavior, and premenstrual syndrome among Chinese female college students. BMC Women's Health, 23(1), 173. https://doi.org/10.1186/s12905-023-02262-x
Solmaz, S., İnan, M., & Şahi̇n, M. (2025). The Moderating Effects of Physical Activity on Social Anxiety and Sleep Disturbance: Managing Gaming Disorder in Young E-Sports Players. Frontiers in Public Health, 13. https://doi.org/10.3389/fpubh.2025.1544044
Tian, Y., Wang, S., Wang, L., & Zhang, Q. (2022). Physical activity and anxiety in college students: The mediating role of mental well-being. Frontiers in psychology, 13, 858983. https://doi.org/10.3389/fpsyg.2022.858983
Tsai, S. Y. (2016). Effect of yoga exercise on premenstrual symptoms among female employees in Taiwan. International journal of environmental research and public health, 13(7), 721. https://doi.org/10.3390/ijerph13070721
Valizadeh, H., & Ahmadi, V. (2021). A causal model of premenstrual syndrome in adolescent girls in Kermanshah County. Disability Studies, 11(1). https://www.sid.ir/paper/1029098/fa
Wang, W. (2025). The Mediating Role of Behavioral Systems in Linking Physical Activity and Anxiety Symptoms in College Students. Scientific reports, 15(1). https://doi.org/10.1038/s41598-025-91294-4
Yorulmaz, Y., Ertarakcı, S., Yıldırım Şahan, Ş., & Turker, T. (2024). Long-term yoga intervention improves premenstrual syndrome, quality of life, and dysmenorrhea: A randomized controlled trial. Health Care for Women International, 45(1), 1-17. https://doi.org/10.1080/07399332.2024.xxxxx
Zehravi, M., Maqbool, M., & Ara, I. (2023). Unfolding the mystery of premenstrual syndrome (PMS): an overview. International Journal of Adolescent Medicine and Health, 35(1), 9-13. https://doi.org/10.1515/ijamh-2022-0023
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2025 Pardis Rahimi (Author); Hassan Abdi (Corresponding Author); Malake Nasery (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.